Flesh-Eating Bacterium Found to Hijack Immune System
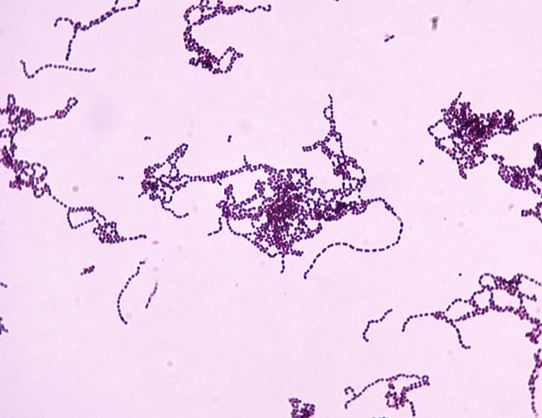
A bacterial pathogen, Streptococcus pyogenes, hijacks the neurons of the immune system in order to promote its own survival, a new study by researchers at the Harvard Medical School has indicated.
Streptococcus pyogenes, the same pathogen that causes strep throat, is the leading cause of serious flesh-eating disease, Necrotizing fasciitis- a severe infection that destroys muscles, skin and underlying tissue.
The word “necrotizing” refers to something that causes body tissue to die. The bacterium digs, burrows deep in the skin and eats into connective tissue and muscle. Furthermore, it is notoriously hard to diagnose and can rapidly become fatal.
“Necrotizing fasciitis is a devastating condition that remains extremely challenging to treat and has a mortality rate that’s unacceptably high,” said study senior investigator Isaac Chiu, assistant professor of microbiology and immunobiology at Harvard Medical School. “Our findings reveal a surprising new role of neurons in the development of this disease and point to promising countermeasures that warrant further exploration.”
Using animal models, the team at Harvard found that a toxin called streptolysin S (SLS), produced by S. pyogenes activated certain pain-related neurons to trigger extreme pain and played a rather interesting role in the ensuing immune-silencing cascade
inside neurons.“Effectively, this neuronal signal silences the alarm system that normally calls on the body’s infection fighters to curb infection,” Chiu said.
In the next round of experiments, the group injected mice with the nerve-blocking substance botulinum neurotoxin A aka the active ingredient in commercial botox. And a week later, these organisms were infected with the disease-causing bacterium. When compared with mice that didn’t receive these nerve-block injections, the aforementioned pre-treated mice developed only minimal wounds- that did not even progress to full-blown disease.
Lastly, scientists blocked neurotransmitter CGRP’s (calcitonin gene-related peptide), immune-suppressing activity with the help of an injectable or ingestible CGRP-blocking molecules. This treatment rendered immune cells immune to the “stop” signal sent by the neurons in case of pain and successfully prevented the spread of necrotizing fasciitis in mice infected with bacterium.
The team says that these consequent results indicate that both the injectable nerve-block approach and drug-based treatments against the neurotransmitter CGRP hold therapeutic promise for necrotizing fasciitis.
“Our findings provide a striking example of how closely intertwined the nervous and immune systems are and how intricate their interaction can be in the setting of infection,” Chiu said. “Our study also underscores the therapeutic potential of modulating one system to affect the other as a way to treat infection.”