Blocking TREM2 Enhance Immunotherapy For Cancers
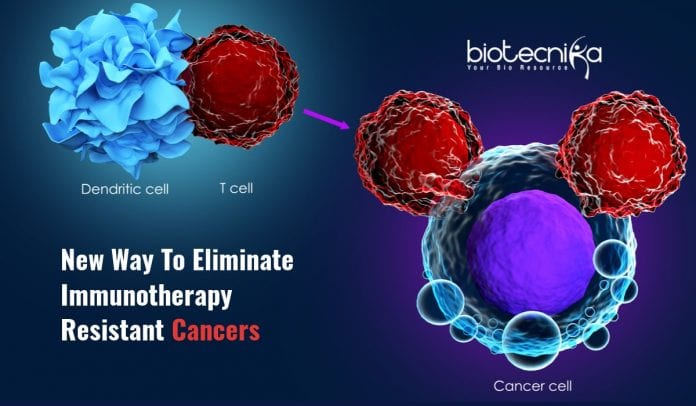
Immunotherapy stimulates the patient’s own immune system to attack cancer cells. It revolutionized the cancer treatment by yielding remarkably quick and complete remission in some cases. Since tumors are notoriously adept at evading immune assault, such drugs work for less than a quarter of patients.
Scientists at Washington University School of Medicine in St. Louis in a new study have now shown that blocking a protein called TREM2 can enhance the effects of standard immunotherapy and can completely eliminate tumors. The study published in Cell on August 11th offers a potential way of making immunotherapy work for more cancer patients.
Rock Belliveau, MD, Professor of Pathology, and Marco Colonna, the senior author of the study, said they had found a new tool to enhance tumor immunotherapy. The growth of certain tumors was reduced by using antibodies against TREM2 alone. They saw a total rejection of the tumor when they combined immunotherapy with TREM2 antibodies. Some antibodies against TREM2 are already in clinical trials for certain other diseases, which is a great thing. The results need to be further verified in animal models. If successful, the scientists will be able to move to clinical trials
easily because there are already antibodies available.Tumor cells can be detected and destroyed by T cells, a kind of immune cells. So tumors create an immune-suppressive environment in and around themselves in order to protect them from T cells and survive. There is an immunotherapy that wakes T cells from their quiescence called checkpoint inhibition, which will stimulate the T cells to attack tumors. But it won’t be enough to eliminate the tumor, it the tumor environment is still immunosuppressive.
Colonna, who is an expert on the immune system, had been studying TREM2 for a long time in the context of Alzheimer’s disease. The TREM2 was linked to underperforming immune cells in the brain. They found that the same kind of immune cells are found in tumors, where they produce TREM2 and inhibits the activity of T cells. They noticed that TREM2 is expressed higher inside te tumor compared to outside, which made it an ideal target for cancer therapy because peripheral tissue will have little effect when they engage TREM2.
They decided to study if blocking TREM2 could boost the tumor-killing powers of T cells by reducing immunosuppression. As a part of this, cancerous cells were injected into mice to induce the formation of sarcoma. They studied four groups of mice; One group received the placebo, one received both checkpoint inhibitor and TREM2 antibodies, one received only checkpoint inhibitor, and the last group received only antibodies against TREM2. The Sarcoma grew steadily in the mice group that received a placebo. They grew more slowly and even disappeared in few cases in mice groups that received either the checkpoint inhibitor or the antibody. Surprisingly, the tumors were completely rejected by those in the mice group that received both. Similar results were obtained with the colorectal cancer cell lines also.
When analyzed the immune cells in tumors of mice that received TREM2 antibody alone, they found that they had very less suppressive macrophages, and the T cells were plenty and active, suggesting that anti-tumor T cell activity can be boosted by blocking TREM2.
Macrophages with TREM2 were found in many kinds of cancers during further experiments. With the help of Cancer Genome Atlas, a publicly available database of cancer genetics, they found that shorter survival in both colorectal cancer and breast cancer is linked to higher levels of TREM2.
To see if TREM2 inhibition is a promising strategy for a range of cancers, they are now expanding their study of TREM2 to other kinds of cancers. Over 200 cases of human cancers and subtypes have shown the expression of TREM2. But they have only tested models of the sarcoma, breast, and colon. There are other models left to test, and they also have to test a mouse model with a human version of TREM2. If that works, they can move to clinical trials.