Blood DNA Methylation Markers Detect Fatal Breast Cancer Up To a Year Earlier
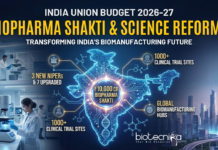
Breast cancer is by far the most frequently occurring cancer in women. Every year 522,000 women die from this type of cancer. Mammography is used as a screening tool for early diagnosis but has its limitations due to over-diagnosis and a modest impact on mortality. The analyses of circulating markers in order to identify women with disseminated disease before diagnosis have not been successful.
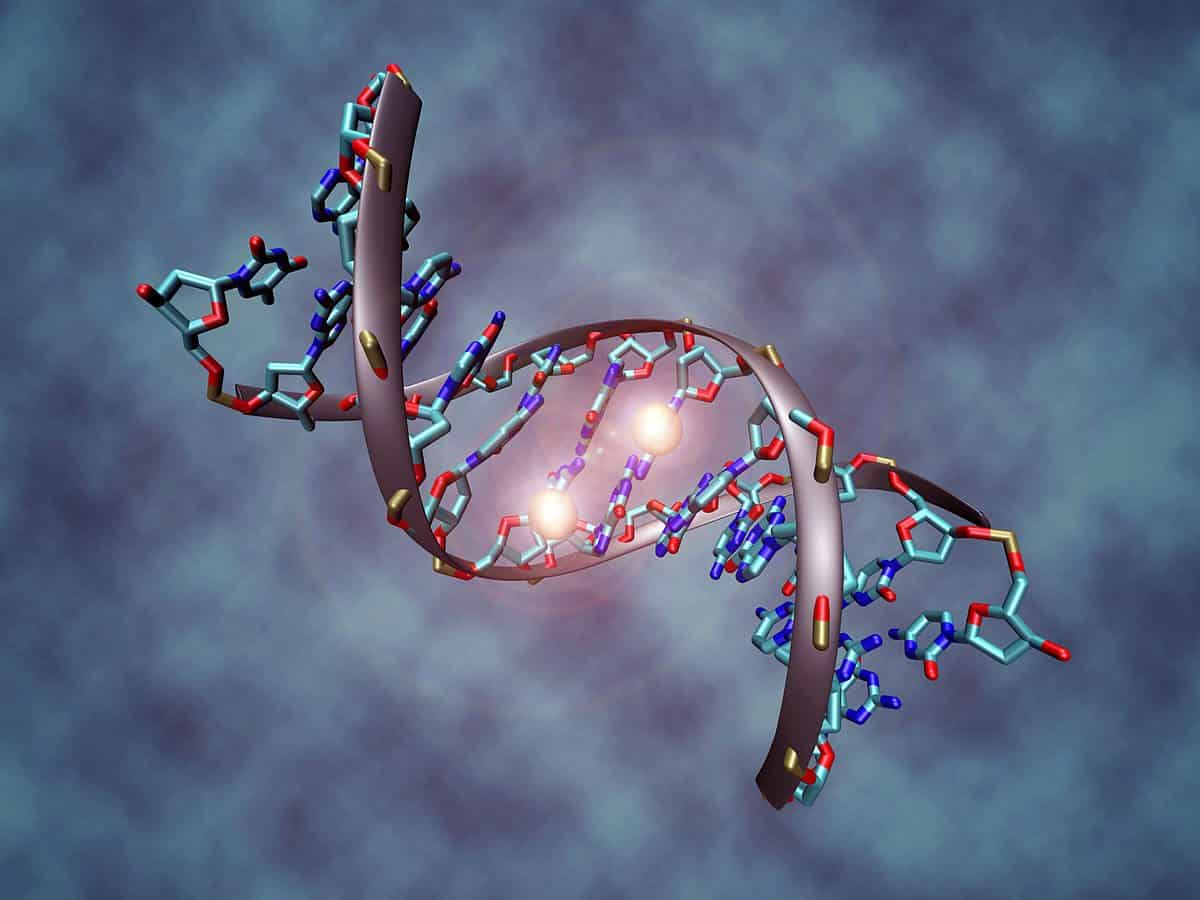
Recently, markers based on DNA shed from tumor cells have shown great promise in monitoring treatment response and predicting prognosis. Over the last decade, DNA methylation (DNAme) has been shown to be a hallmark of cancer and occurs very early in breast cancer development. DNAme is centered around specific regions (CpG islands) and is chemically and biologically stable. This enables the development of early detection tools and personalized treatment, based upon the analysis of cell-free DNA contained within serum or plasma.
In this direction, scientists at the University College London have now identified a new marker that could be used to diagnose fatal breast cancer up to one year ahead of current methods.
A team of researchers found that in breast cancers small molecules of carbon and hydrogen become attached to EFC#93 in a process called DNA methylation. Abnormal DNA methylation is common in human tumours and methylation changes occur very early in breast cancer development.

Professor Martin Widschwendter said: “We found that the presence of EFC#93 DNA methylation in blood serum correctly identified 43% of women who went on to be diagnosed with fatal breast cancers within three to six months of giving serum samples, as well as 25% of women who went on to be diagnosed within six to twelve months of giving samples.”
In the course of the study, the team used blood serum samples from almost 1,000 women, researchers looked for the presence of carbon and hydrogen molecules attached to a chunk of DNA called EFC#93. The method helped to identify cancer in 43 percent of women who were diagnosed six months later.
To assess whether EFC#93 can diagnose women with a poor prognosis earlier (that is, before the cancer becomes detectable) the authors further analysed serum samples of 925 healthy women, 229 of whom went on to develop fatal and 231 of whom went on to develop non-fatal breast cancer, within the first three years of donating serum samples.
Professor Widschwendter said: “The serum DNA methylation marker EFC#93 correctly identified 43% of women from serum tested six months in advance of their mammography-based breast cancer diagnosis who later died from the disease (sensitivity for fatal breast cancer) and also identified 88% of women who did not go on to develop breast cancer (specificity).
“Importantly, EFC#93 did not detect non-fatal breast cancers early. In comparison, mammography screening has a specificity of 88-92% but leads to very substantial over-diagnosis, which means that tumours are detected that would never have caused any clinical symptoms. Subject to further study, using cell-free DNA as a marker, as we have done here, is a promising way of avoiding this issue. ”
Clinicians are following up on the study, published this month in the journal Genome Medicine, to see if hormone therapy could preemptively help women who have DNA methylation at EFC#93 but haven’t received a positive diagnosis through mammography.
“For the first time, our study provides evidence that DNA methylation markers such as EFC#93 provide a highly specific indicator that could diagnose fatal breast cancers up to one year in advance of current diagnosis,” Widschwendter said. “This may enable individualized treatment, which could even begin in the absence of radiological evidence in the breast.“