A Glitch in T cell Regulatory Pathway Could Contribute to MS
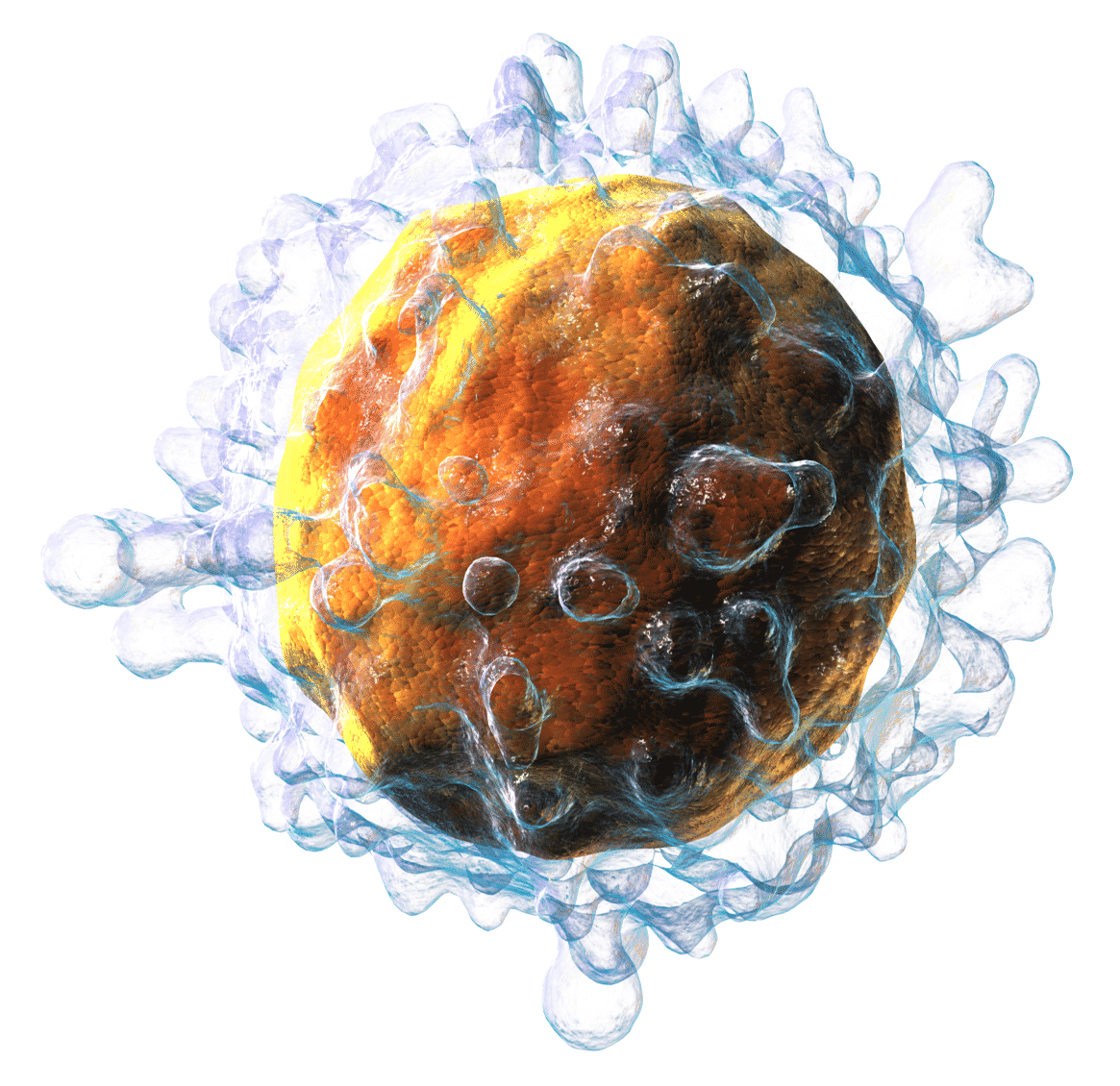
Multiple sclerosis (MS), a neurological disease that affects an estimated 2.3 million people, occurs when the immune system attacks the myelin sheath, the protective coating that encases nerve cells, triggering symptoms such as vision problems, poor balance, and muscle spasms.
Today’s MS drugs work mainly by tightening the leash on the immune system. Current treatments typically kill all immune cells, which prevents them from ravaging myelin but also leaves the body vulnerable to infection.
Now, however, a University of the Edinburgh-led team headed by Siobhan Ni Choileain have pinpointed a “glitch” in the T cells of MS patients that sabotaged the processing of the protein CD46, which controls the conversion of helper T cells into Tregs. In healthy cells, the stimulation of a T-cell receptor led to the glycosylation of CD46, which did not happen in cells isolated from MS patients, they found.
One of the hallmarks of autoimmune diseases, such as multiple sclerosis (MS), is the lack of regulatory T cells to suppress inflammation. Regulatory T cells play an important role in the immune system: They rein in wayward T cells that attack normal tissues in the body, causing autoimmune
diseases like multiple sclerosis.Ligation of the complement regulatory protein CD46 facilitates the differentiation of T helper 1 (TH1) effector cells into interleukin-10 (IL-10)–secreting type 1 regulatory T cells (Tr1 cells), and this pathway is defective in MS patients. Cleavage of the ectodomain of CD46, which contains three N-glycosylation sites and multiple O-glycosylation sites, enables CD46 to activate T cells.
The investigators found that stimulation of the T cell receptor (TCR)–CD3 complex was associated with a reduction in the apparent molecular mass of CD46 in a manner that depended on O-glycosylation. CD3-stimulated changes in CD46 O-glycosylation status reduced CD46 processing and subsequent T cell signaling.
During the course of the study, for the sake of T cell activation, CD46 was recruited to the immune synapse in a manner that required its serine-, threonine-, and proline-rich (STP) region, which is rich in O-glycosylation sites. Recruitment of CD46 to the immune synapse switched T cells from producing the inflammatory cytokine interferon-γ (IFN-γ) to producing IL-10.
Furthermore, CD4+ T cells isolated from MS patients did not exhibit a CD3-stimulated reduction in the mass of CD46 and thus showed increased amounts of cell surface CD46.
The findings may explain why this pathway is faulty in patients with MS and provide clues as to how the disease develops. They could inspire the development of immunotherapies against the neurodegenerative disease.