COVID-19 Infection Pattern Studied By UNC Scientists
The researchers across the globe are working round the clock to understand more about the new deadly disease COVID-19. But, more insights into the progression and severity of the disease can be understood if the cells that support the infection and the extent of infection can be studied.
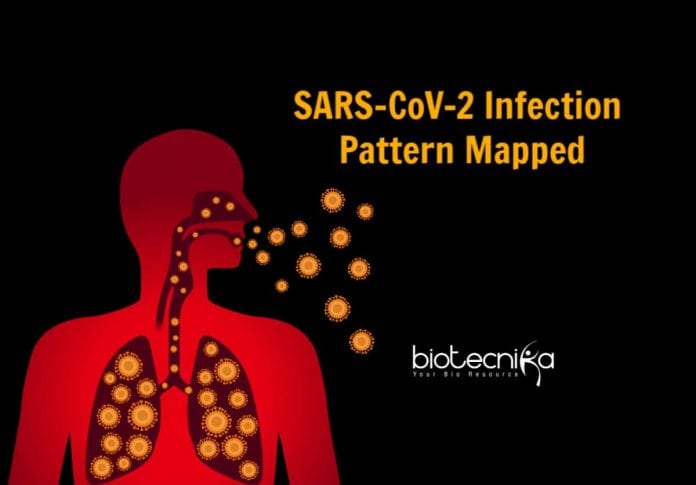
The UNC School of Medicine scientists decided to study which cells in the respiratory airway are infected by the virus and how the novel coronavirus gets into the lungs of patients who develop pneumonia.
They were able to understand some of the ways in which the novel coronavirus infects nasal cavity and infects and replicates progressively less well in cells lower down the respiratory tract—including the lungs.
They discovered that the virus first firmly establishes in the nasal cavity, and some times they get aspirated into the lungs where they cause more serious diseases like pneumonia.
The researchers published their results in Cell. According to Richard Boucher, author of the paper, masks that protect nasal passages, and therapeutic strategies that reduce the virus in the nose like antiviral nasal sprays or nasal irrigation could be beneficial, if the dominant initial site of infection of the
virus is the nose.Ralph Baric, Ph.D., professor of epidemiology at the UNC Gillings School of Public Health, said this is a landmark study that reveals unexpected insights into the mechanisms that regulate disease progression and severity following SARS-CoV-2 infection.
The researchers developed a new reverse genetic platform for the novel coronavirus that helped them produce key indicator viruses that will support the vaccine development for COVID-19. They developed a GFP reporter virus to explore SARS-CoV-2 pathogenesis, using a reverse genetics system.
Using high-sensitivity RNA in situ mappings, they mapped the COVID-19 infection pattern in respiratory tracts. They discovered that ACE2 is highly expressed in the nose, and its expression decreases throughout the lower respiratory tract. ACE2 is the cell surface receptor the SARS-CoV-2 viruses use to get into the cells.
To confirm their findings, they observed how efficiently different isolates of SARS-CoV-2 could infect cultured cells from different parts of the human airway. And they found a striking pattern of gradient from relatively high infectivity of SARS-CoV-2 in cells of nasal passages, to less infectivity in cells of the throat and bronchia, to relatively low infectivity in lung cells.
They also studied two protein-cleaving enzymes, furin, and TMPRSS2 found on human cells that help SARS-CoV-2 viruses to enter human cells by reshaping key virus proteins. The viruses have increased the ability to infect cells and replicate where these human enzymes are more abundant.
Researchers noticed that the SARS-CoV-2 virus did not infect club cells that line the airways though they express both ACE2 and TMPRSS2. And the same type of airway cells from different individuals had significantly varied susceptibility to infection. This suggests that there are factors yet to be discovered that determine the extent of infection in individuals.
The people at higher risk for severe lung disease—the elderly, obese, and diabetic—are more prone to aspiration, especially at night, is consistent with the hypothesis that aspiration of oral contents into the lung is a significant contributor to COVID-19 pneumonia.
They also found that previously identified neutralizing antibodies for the MERS 2012 and SARS of 2002, did not neutralize the novel coronavirus SARS-CoV-2. However, two of five SARS 2002 patients’ blood serum had a low level but significant capability to neutralize the novel coronavirus in cultured cells. These studies show that people exposed to other types of coronaviruses might have partial protection against SARS-CoV-2, as they carry some other types of antibodies in their blood.
These studies of COVID-19 infection pattern in respiratory tracts open new directions for future studies on SARS-C0V-2 that could help develop treatments or practices to reduce the severity and transmission of COVID-19.