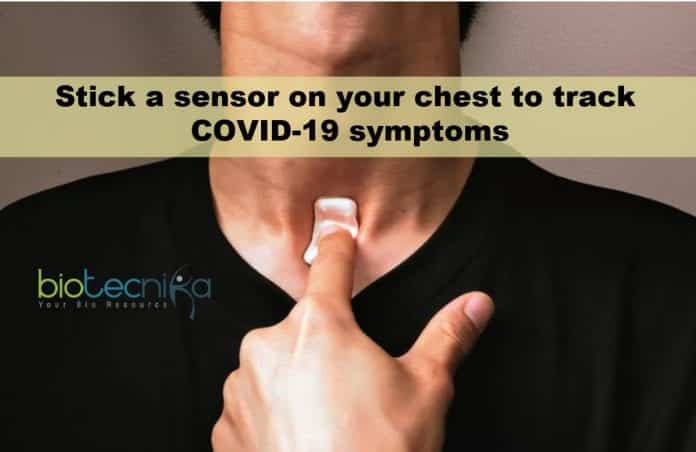
Stick a sensor on your chest to track COVID-19 symptoms
This sensor device checks for the onset and development of COVID-19 infection by detecting the nature, duration, and time of coughs.
The device appears like a Band-Aid, but it’s a flexible wireless sensing unit that sits where your throat and chest meet, sensing coughing and breathing problems related to COVID-19 infection. The system, revealed on Monday, can check early symptoms of coronavirus infection and the development of the disease.
It has been developed by Northwestern University and the Shirley Ryan AbilityLab in Chicago – which hard-hit by the deadly virus. It adheres to the little well at the base of your throat – the skin below your suprasternal notch – where air movement is closest to the skin and where tracheostomies are carried out. This non-invasive patch relates to a sensing unit for monitoring speech as well as swallowing in patients recovering from strokes. This sensor model was tuned to track COVID-19 symptoms including coughing and breathing issues that are main to COVID-19 infection.
“Microphone is not used as there are troubles with microphones with ambient noise and also tremendous intrusions of personal privacy. We utilize a high-bandwidth, tri-axis accelerometer
to gauge the movement of the surface area of the skin to get the details of coughing as well as breathing and not unlike a digital stethoscope, said Professor John Rogers, Director, Northwestern University’s Center on Bio-Integrated Electronics said.Additionally, the device detects heart rate as well as temperature level.
The patch has to be peeled off once a day and place it on a wireless charger, which syncs the stored data to an iPad nearby. The data from here is uploaded to a HIPAA-compliant cloud where an exclusive AI algorithm analyzes it for anomalies associated with COVID-19 infection. Its easier to disinfect the gadget as it has no external ports for connectivity or power.
Artificial Intelligence has taken something of beating lately for promising supply in health diagnosis which is more than it could offer.
John Rogers said, “We like AI, but we’re not wedded to it and we are wedded to things that work”. “We make use of digital filtering algorithms that search the data for specific signatures. We’re seeking fads, not an outright gold standard measurement. And we have an understanding of physics underlying”.
During the onset, the data is confirmed by a skilled human prior to any indications are sent to medical professionals. 25 test subjects have been using the device for 2 weeks until now, producing 1,500 hours of history and one terabyte of information.
The missing thing from the sensor patch is a blood oxygen perfusion sensing unit, but Rogers says that is can be found in the near future. To measure oxygen perfusion – Fingertip pulse oximeters, are the current personal health product to be snapped up after some records suggested that low blood oxygen was an initial characteristic of COVID-19 infection.
Presently, dozens of new patches are being produced per week by a lab at Northwestern’s Chicago campus. It has the capability to scale to hundreds of devices a week before making the patch available for large scale manufacturing using the license.
The COVID-19 sensor of Northwestern University joins an array of activity trackers, blood pressure, and glucose monitors that suggest we’ll quickly put on a clinics’ worth of medical sensors to get in front of health problems before they transform into a severe situation.
Rogers said, “I think that needs a hardware platform that is virtually hard to sense”. “When you move from anecdotal tracking of status to continuous, healthcare as a whole will be improved. I have always assumed that makes sense”.
Author: Sruthi S