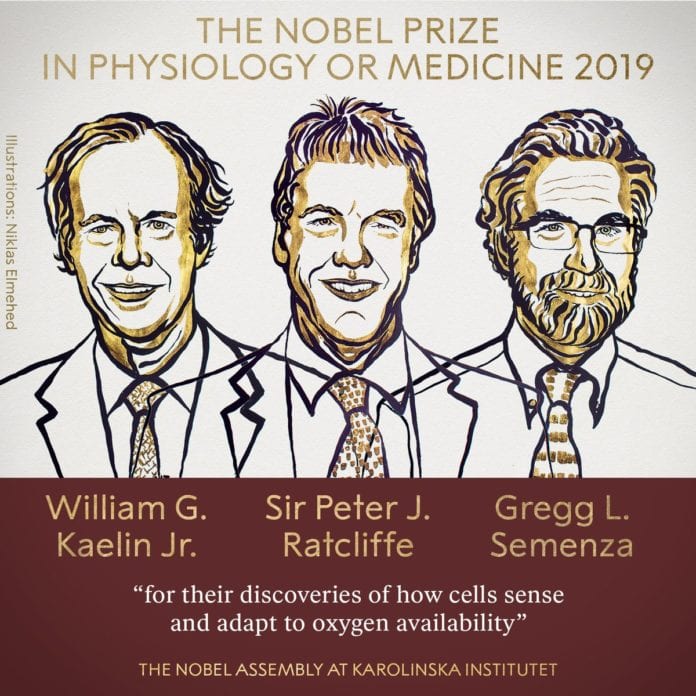
Nobel Prize in Medicine 2019 Awarded for Research on How Cells Manage Oxygen
The Nobel Assembly at Karolinska Institutet, on Monday, has decided to award the Nobel Prize in Physiology/Medicine for the year 2019, jointly to William G. Kaelin Jr., Gregg L. Semenza, and Sir Peter J. Ratcliffe for their studies and discoveries of how cells sense & adapt to oxygen availability.
Their research work established the genetic mechanisms that allow cells to respond to changes in oxygen levels. The findings have implications for treating a variety of diseases, including cancer, anemia, heart attacks, and strokes.
Animals need oxygen for converting their food into useful energy. The fundamental importance of oxygen in the living has been understood for centuries; Still how cells adapt to the changes in levels of oxygen has been unknown until this discovery.
William G. Kaelin Jr., Gregg L. Semenza, and Sir Peter J. Ratcliffe discovered how the cells can sense & adapt to the changing oxygen availability. The team identified the molecular machinery that regulates the activities of genes in response to the varying levels of oxygen.

Seminal discoveries by this year’s Nobel Laureates have revealed the mechanism for one of life’s most essential adaptive processes. The team established the basis of how oxygen levels affect cellular metabolism & physiological function. These discoveries have also paved the way for promising new strategies to fight anemia, cancer & many other diseases.
Oxygen makes up about one-fifth of our Earth’s atmosphere. O2 is essential for animal life. Oxygen is used by the mitochondria organelle present in virtually all animal cells in order to convert their food into useful energy. Otto Warburg, the 1931 Nobel Prize in Physiology or Medicine recipient, revealed that this conversion is an enzymatic process.
Watch the very moment the 2019 Nobel Prize in Physiology or Medicine is announced.
Presented by Thomas Perlmann, Secretary of the Nobel Committee.#NobelPrize pic.twitter.com/LFswOT24AJ
— The Nobel Prize (@NobelPrize) October 7, 2019
During the evolution, mechanisms developed to ensure a sufficient supply of O2 to tissues and cells. The carotid body which is adjacent to large blood vessels on both sides of the neck contains the specialized cells that sense the blood’s O2 levels. The 1938 Nobel Prize in Physiology/ Medicine to Corneille Heymans awarded discoveries showing how blood O2 sensing via the carotid body controls the respiratory rate by communicating with the brain directly.
And in addition to the carotid body controlled rapid adaptation to low O2 levels (hypoxia), there are other fundamental physiological adaptations too. The key physiological response to hypoxia is the rise in levels of the hormone erythropoietin (EPO) which actually leads to the increased production of RBCs (erythropoiesis). The importance of hormonal control of erythropoiesis hormone was already known by the beginning of the 20th century, but how this process was itself controlled by Oxygen remained a mystery.
Gregg Semenza studied the hormone erythropoietin gene & how it is regulated by varying O2 levels. By using the gene-modified mice, specific DNA segments located next to the erythropoietin gene were shown to mediate the response to hypoxia. Sir Peter Ratcliffe also studied Oxygen-dependent regulation of the hormone erythropoietin gene,& both research groups found that the O2 sensing mechanism was present in virtually all tissues, not only in the kidney cells where hormone erythropoietin is normally produced. These were some of the important findings that came up, showing that the mechanisms were general & functional in many different cells and their types.
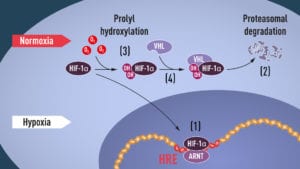
Semenza had wished to identify the cellular components that are mediating this response. In the cultured liver cells, he actually discovered a protein complex that can bind to the identified DNA segment in an O2-dependent manner. Semenza called this complex as a hypoxia-inducible factor (HIF). Extensive efforts to purify the hypoxia-inducible factor complex began in 1995 and Semenza was able to publish some of his study key findings, including identification of the genes encoding Hypoxia-Inducible Factor. The HIF was found to consist of 2 different DNA-binding proteins, so-called transcription factors, now named hypoxia-inducible factor HIF-1α & ARNT. The research team could begin solving the puzzle, allowing them to understand which are the additional components that were actually involved & how the machinery works.
When O2 levels are high, cells contain very little HIF-1α. However, when O2 levels are low, the amount of HIF-1α increases so that it can bind to and thus regulate the hormone erythropoietin gene as well as other genes with HIF-binding DNA segments. Several research teams showed that HIF-1α, which is normally rapidly degraded, is protected from degradation in hypoxia. At normal O2 levels, a cellular machine called the proteasome, recognized by Aaron Ciechanover, Avram Hershko and Irwin Rose-the 2004 Nobel Prize in Chemistry-, degrades HIF-1α. And under such conditions, a small peptide called ubiquitin is actually added to the HIF-1α protein. The ubiquitin peptide functions as a tag for proteins destined for degradation in the proteasome. How ubiquitin binds to HIF-1α in an O2-dependent manner remained a central question.
The answer to this came from an unexpected direction. At about the same time as Semenza & Ratcliffe were exploring the regulation of the hormone erythropoietin gene, cancer researcher William Kaelin, Jr. was studying on an inherited syndrome, von Hippel-Lindau’s disease (VHL disease). This genetic disease leads to a dramatically increased risk of certain cancers in families with inherited VHL mutations. Kaelin showed that von Hippel-Lindau’s disease gene encodes a protein that can prevent the onset of cancers. Kaelin also showed in the study that the cancer cells lacking a functional von Hippel-Lindau’s disease gene express abnormally high levels of the hypoxia-regulated genes. But that when the von Hippel-Lindau’s disease gene was reintroduced into the cancer cells, normal levels were actually restored. This was an important clue showing that von Hippel-Lindau’s disease gene was somehow involved in controlling the responses to hypoxia. And some additional clues came from several research groups showing that von Hippel-Lindau’s disease gene is part of a complex that labels the proteins with ubiquitin, marking the proteins for degradation in the proteasome. Ratcliffe and his research team then made a key discovery: which demonstrates that VHL can physically interact with the HIF-1α gene and it is required for its degradation at normal oxygen levels. This conclusively linked VHL to HIF-1α.
Many pieces had actually fallen into place, but what was still lacking was an understanding of how oxygen levels regulate the interaction between VHL & HIF-1α genes. The search was focused on a specific portion of the HIF-1α protein known to be important for VHL-dependent degradation, & both Kaelin and Ratcliffe suspected that the key to Oxygen sensing resided somewhere in this protein domain. In the year 2001, in two simultaneously published articles the team showed that under normal O2 levels, hydroxyl groups are added at 2 specific positions in HIF-1α. This protein modification is called prolyl hydroxylation and it allows the VHL gene to recognize & bind to the HIF-1α gene and thus explained how the normal oxygen levels control rapid HIF-1α degradation with the help of O2-sensitive enzymes (so-called prolyl hydroxylases). Further studies by Ratcliffe & others identified the responsible prolyl hydroxylases. It was shown that the gene activating the function of the HIF-1α gene was regulated by O2-dependent hydroxylation. The Nobel Laureates had elucidated the oxygen sensing mechanism & had shown how it works.
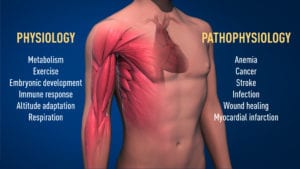
Thanks to the groundbreaking research work of these Nobel Laureates, we know much more about how different O2 levels regulate fundamental physiological processes. O2-sensing allows cells to adapt their metabolism to low O2 levels: for example, in our muscles during intense exercise. Other examples of adaptive processes controlled by O2 sensing include the generation of new blood vessels & the production of RBCs. Our immune system & many other physiological functions are also fine-tuned by the Oxygen-sensing machinery. O2 sensing has even been shown to be essential during fetal development for controlling normal blood vessel formation and placenta development.
O2 sensing is central to a large number of diseases. For example, patients with chronic renal failure often suffer from severe anemia due to decreased hormone erythropoietin expression. Hormone erythropoietin is produced by cells in the kidney and is essential for controlling the formation of red blood cells, as explained above. Moreover, O2-regulated machinery has an important role in cancer. In tumors, the O2-regulated machinery is utilized to stimulate blood vessel formation & to reshape metabolism for effective proliferation of cancer cells. The intense ongoing efforts in academic labs & pharmaceutical companies are now focused on developing drugs that can actually interfere with the different disease states by either activating/ blocking, the O2-sensing machinery.
Editor’s Note: Nobel Prize in Medicine 2019. William G. Kaelin Jr., Gregg L. Semenza, and Sir Peter J. Ratcliffe. Discoveries on how cells sense & adapt to oxygen availability.