Breakthrough Discovery : Self-Renewing Pluripotent Stem Cells Created
In a breakthrough discovery, Researchers at UCLA have successfully created a Renewable Source Of Cancer Fighting T cells. A novel technique for coaxing pluripotent stem cells has been developed. Pluripotent stem cells are the ones responsible for producing each cell type in our body and now using this technique it can be grown indefinitely in the lab. Under this technique, artificial thymic organoids were used that mimic the functionality of naturally occurring Thymus gland – where T cells are formed from Blood stem cells. This could revolutionize the way cancer is treated.
T cells, fight infections in our body and also have the potential to kill cancerous tumor cells. Self-renewing pluripotent stem cells by this technique developed by UCLA scientists can open up new doors for cancer immunotherapy and T cell therapies for viral infections such as HIV, and other autoimmune diseases. Moreover, this technique can be used in combination with gene editing approaches to create a virtually unlimited supply of T cell, that can be supplied on a large scale to the needy patient, thus eliminating the need to use a patient’s own T cells for therapies.
The study was published in Cell Stem Cell journal and was led
by senior author Dr. Gay Crooks, a professor of pathology and laboratory medicine and of pediatrics and co-director of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA.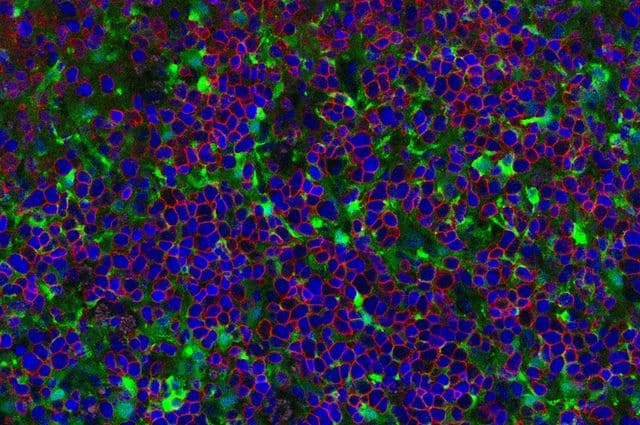
Image Courtesy: UCLA Broad Stem Cell Research Center/Cell Stem Cell
Currently used T cell therapies have huge potential to treat different cancer forms. It involves collecting T cells from a patient, genetically engineering them with a receptor to recognize and destroy cancer cells, and then infusing the cells back into the patient. But in most of the cases the genetically engineered T cells don’t function well and also the treatment is heavy on the pockets of patients. This new technique developed is designed to be more accessible and affordable apart from being super effective.
Crooks – director of the Cancer and Stem Cell Biology Program at the UCLA Jonsson Comprehensive Cancer Center along with her team previously demonstrated that the 3D structure of an artificial thymic organoid allowed mature T cells to develop from adult blood stem cells, and hypothesized that they would also support mature T cell production from pluripotent stem cells.
As per the study, the artificial thymic organoids can efficiently produce mature T cells from both kinds of pluripotent stem cells namely: embryonic stem cells, which originate from donated embryos and induced pluripotent stem cells. The team could also genetically engineer pluripotent stem cells to express a cancer-targeting T cell receptor and, using artificial thymic organoids, generate T cells capable of targeting and killing tumor cells in mice.
The challenge faced by the UCLA researchers now is that the T cells generated from the artificial thymic organoids have a lining of additional unknown molecules on their surface that may not match to individual patients, this could lead the patient’s body to reject the cells that will be transplanted.
“Our next step will be to create T cells that have the receptors to fight cancer but do not have the molecules that cause the rejection of the cells, which would be a major step toward the development of universal T cell therapies,” said Dr. Christopher Seet, the study’s first co-author and a clinical instructor in the division of hematology-oncology at UCLA in their press release.
The license for the artificial thymic organoid method for cancer therapy currently is in possession by Kite, a Gilead Company and is patented by the Regents of the University of California. FDA is yet to approve this technique for human clinical trials.