CRISPR Facilitates Successful Red Blood Cell Transfusion
Popular simplification of blood groups while collection of blood at hospitals and centres has led to the misrepresentation of the complexity of RBC surface antigens that influence donor–recipient compatibility with 36 blood group systems and more than 350 different antigens recognised by the International Society of Blood Transfusion.
Mismatch of any blood group antigen has the potential to cause alloimmunisation (generation of antibodies to non‐self RBC antigens). Across all transfusion recipients, this occurs in approximately 2–5% of cases; however, in chronically transfused sickle‐cell disease (SCD) patients, RBC alloimmunisation occurs in approximately 30% of cases.
Whilst alloimmunisation of chronically transfused patients increases the difficulty in obtaining suitably matched donations, individuals exist with non‐pathological but particularly rare naturally occurring blood group phenotypes that also present major challenges for blood transfusion services across the world to match.
The ability to generate RBCs with bespoke phenotypes for individuals with rare blood types together with a “more universal” source of RBCs designed to minimise alloimmunisation in SCD patients and to meet the transfusion needs of existing patients for whom alloimmunisation has reduced the suitable donor pool would have obvious clinical benefits.
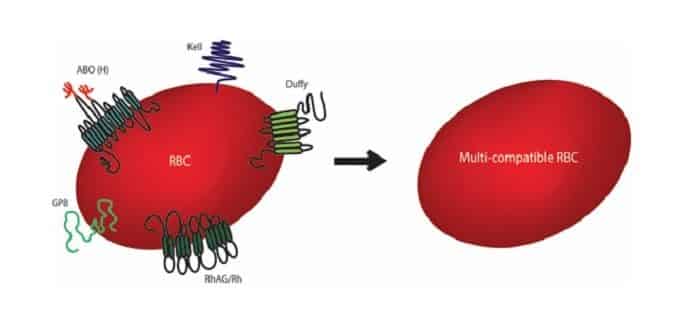
The desire to improve RBC compatibility for transfusion is not a new concept. Now, scientists at the U.K.-based NIHR Blood and Transplant Research Unit (NIHR BTRU) in red cell products, BrisSynBio Center, and NHS Blood and Transplant in Bristol have developed individual cell lines in which specific blood group genes were altered using CRISPR to prevent the expression of blood group proteins that can cause immune reactions.
Dr. Ashley Toye Director of the Bristol NIHR BTRU said: “Blood made using genetically edited cells could one day provide compatible transfusions for a group of patients for whom blood matching is difficult or impossible to achieve within the donor population. However, much more work will still be needed to produce blood cells suitable for patient use.”
The study is the first that demonstrate the use of gene editing in combination with laboratory culture of red blood cells to generate rare or customized red blood cells for patients with specific needs. While the authors stress the many challenging technical obstacles that must be overcome before this approach could be translated to a clinical product, they believe their work does provide a window into the possible applications of red blood cells produced from gene-edited cell lines.






























