Taking a Breather- Brain Organoids Make Themselves at Home in Mice Models
Differentiation of human pluripotent stem cells to small brain-like structures known as brain organoids offers an unprecedented opportunity to model human brain development and disease.
Brain organoids grown in culture dishes or test tubes are structurally and functionally limited because, without a system of blood vessels, nutrients cannot reach the interior of their 3D structure. This reduces organoids’ survival time and complexity, as cells cannot undergo as many divisions to increase their number or to diversify cell type.
Although some researchers have attempted to address these limitations by simultaneously grafting vascular tissue onto organoids, this approach still does not fully mimic the cellular microenvironment of an actual brain.
Also, when you build models, whether ships or cars, you want them to be as much like the real deal as possible. This quality is even more crucial for building model organs, because disease treatments developed from these models have to be safe and effective for humans.
In this direction, scientists at the Salk Institute developed a vascularized and functional in vivo model of brain organoids, and to both their surprise and shock, found that these grafts exhibiting progressive neuronal differentiation and maturation, gliogenesis, integration of microglia, and growth of axons to multiple regions of the host brain.
“Brain organoids are powerful tools for investigating human brain development and disorders,” says senior author Rusty Gage, professor of Salk’s Laboratory of Genetics. “But currently they do not fully represent native physiological environments. This work brings us one step closer to a more faithful, functional representation of the human brain and could help us design better therapies for neurological and psychiatric diseases.”
Study coauthor Fred “Rusty” Gage, a neuroscientist at the Salk Institute for Biological Studies in La Jolla, California, and his colleagues first started thinking about the health of brain organoids a few years ago when they began working with the structures.
Gage’s team used human pluripotent stem cells to develop brain organoids, which were grown in culture for 40 to 50 days. Then, the team inserted the organoids into cavities made in mice’s retrosplenial cortex—a region critical for movement and spatial learning. The mice had “humanized” immune systems, Gage says, meaning that their immune cells had been engineered not to attack human tissue.
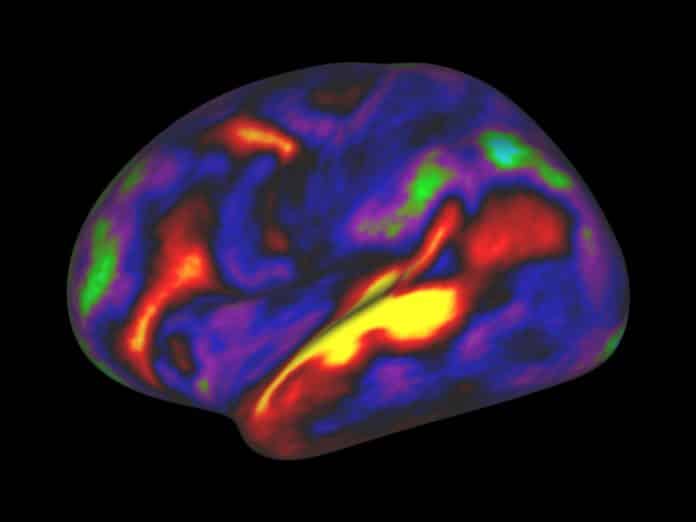
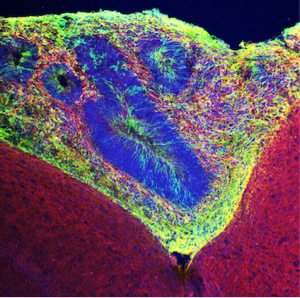
Around day 5 after transplantation, blood vessels in the organoids could be detected using a fluorescent dye, and by day 14 an extensive network of vessels had grown deep within the human tissue graft.
Within two to 12 weeks, the organoids were sprouting additional neurons, including ones found in very specific regions of the human cortex; glia cells including astrocytes; and neural stem cells. By 14 days almost all the organoids had developed a rich network of blood vessels carrying nutrients and oxygen, allowing them to survive for up to 233 days. Their structure and cell maturation was that of a newborn.
The implanted organoids were also sending axons — the biological wires that carry brain signals from one neuron to another — into both sides of the mouse brain, not only the side with the window, and forming such strong synapses with mouse neurons that the neural activity of the two species was synchronized.
“When neurons fire together, that means they are connected and [engage in] cross-talk,” said Salk’s Abed Mansour, the paper’s lead author, forming “neuronal networks.”
Crucially, the team didn’t fail to acknowledge the ethical elephant in the room: No, they insist, the mice didn’t suddenly become smarter or more human-like as a result of the human neurons entwining with their own.
While ethical questions continue to arise alongside the advances being made in human brain-to-mouse research, scientists hope that the organoids will expand their understanding of how to repair myriad neurological conditions, including brain injuries, dementia, and strokes. Given how new this research is, though — there is a lot left to discover in terms of how the organoid transplants will affect medical studies moving forward, and also the mice serving as tiny vehicles of such discovery.