CRISPR Employed Outside Cell for the First Time
The possibility of rewriting the genome of an organism, or even of an entire species, has long been the stuff of science fiction. And with CRISPR, fiction has edged closer to reality. CRISPR exploits an ancient system that allows bacteria to acquire immunity from viruses. It uses an enzyme called Cas9 to cut strands of DNA at precisely targeted locations, allowing researchers to insert new genetic material into the gap. But—at least until now—all of that cutting and pasting has gone on inside cells.
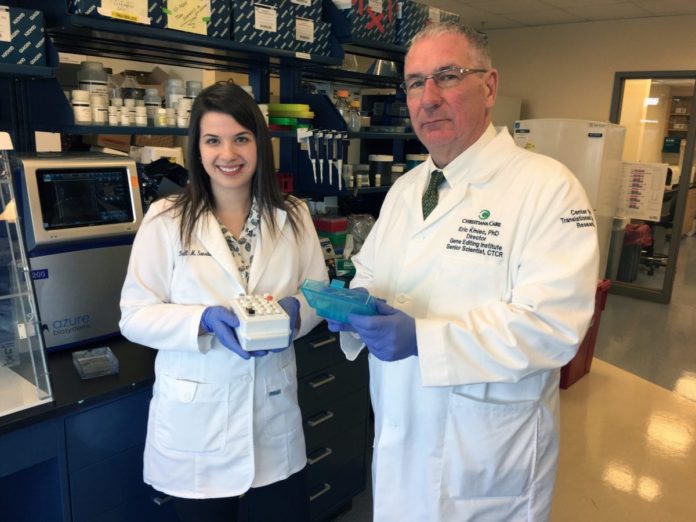
Now, researchers from Christiana Care Health System used CRISPR to edit DNA outside the cell, laying the groundwork for a diagnostic test that can replicate DNA mutations in a patient’s tumor and help physicians identify the most appropriate treatment.
The team says their new “cell-free” CRISPR technology is the first CRISPR tool capable of making multiple edits to DNA samples “in vitro,” which means in a test tube or petri dish.
The advance could have immediate value as a diagnostic tool, replicating the exact genetic mutations found in the tumors of individual cancer patients.
“With this new advance, we should be able to work with laboratory cultures and accomplish gene edits in less than a day, significantly reducing the time required for diagnostics compared to other CRISPR tools, and with much greater precision,
” said Eric Kmiec, Ph.D., director of the Gene Editing Institute and principal author of the study. “This is particularly important for diagnostics linked to cancer care where time is critical.”“When you’re working with CRISPR inside a cell, you’re kind of working in a black box where you can’t really observe the gears of the machinery that are doing these amazing things,” Eric Kmiec, lead researcher and director of the Gene Editing Institute, said. “You can see the results, the edits to the genes, but not necessarily how you got there, which is important for ensuring that CRISPR can be safely used to treat patients.”
To create a “cell-free” CRISPR tool, Kmiec and his colleagues replaced Cas9 with another protein: Cpf1, also known as Cas12a. With CRISPR-Cpf1, they found they could remove a molecule of DNA- the plasmid from a cell and edit it in a test tube. When Cas9 cuts DNA, the result can be “blunt ends,” while Cpf1 produces “sticky ends.” The blunt-ended outcome could impede the ability to process the cut ends, which allows for the removal or “resection” of a section of genetic code and then seamlessly insert and attach new code.
The Gene Editing Institute is now working to use the new CRISPR-Cpf1 breakthrough to provide something akin to CRISPR on a computer chip to a commercial partner involved in cancer diagnostics that is intended to drive personalized cancer care.