CRISPR a Solution to Inherited Blood Disorders: Study
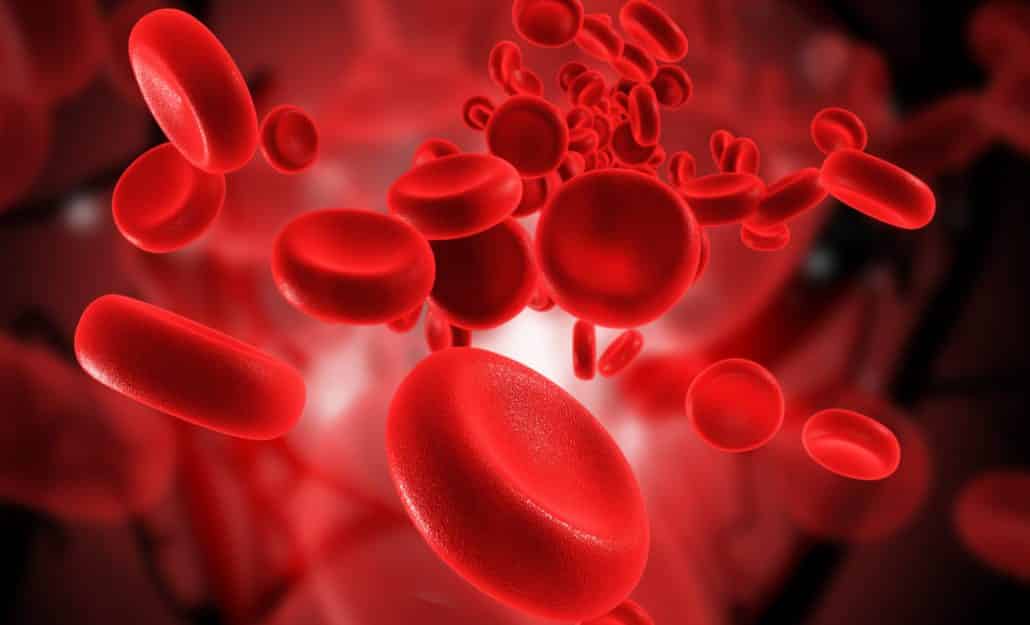
Sickle cell is essentially caused by a typo in the instructions for making the protein haemoglobin, which is densely packed into red blood cells. Sickle cell disease causes normally round red blood cells, which carry oxygen around the body, to become shaped like a sickle. These deformed cells can lock together to block the flow of blood around the body. This can cause intense pain, organ damage and can be fatal.
Now, a University of South Wales, Sydney-led study has determined how naturally-occurring gene mutations can counter the effects of inherited blood diseases. This, in turn, has opened the potential to use gene editing to treat patients with sickle cell disease, thalassemia, and other disorders.
Humans express different forms of hemoglobin genes at different developmental stages, the authors explain. The early human embryo expresses embryonic globin genes; then there is a switch to producing a fetal form of hemoglobin, and at around the time of birth production is switched again from the fetal to the adult form of hemoglobin. Adult humans generally only produce only about 1% residual fetal hemoglobin. However, some individuals have a rare, benign condition known as hereditary persistence
of fetal hemoglobin (HPFH), which means that they continue to produce fetal hemoglobin into adulthood.For patients with HPFH who also have ß-hemoglobinopathies, such as sickle cell disease or ß-thalassemia, this continued production of fetal hemoglobin reduces the severity of their disease because the extra fetal hemoglobin compensates for the lack of adult hemoglobin.
The ability to trigger production of fetal hemoglobin intentionally therefore represents a “therapeutic goal” for widespread treatment of blood disorders, the team states. “The fetal hemoglobin gene is naturally silenced after birth,” comments Dr. Crossley. “For 50 years, researchers have been competing furiously to find out how it is switched off, so it can be turned back on.”
The scientists used gene editing to introduce the mutations into blood cells as a way to boost fetal hemoglobin production. The mutations that cause the disorders are naturally carried by a small percentage of people, but the highly individualized method could help treat some of them.
The two genes that switch off the fetal hemoglobin gene by binding directly to it are called BCL11A and ZBTB7A.
Later, after this discovery, the scientists turned their attention to using the gene-editing technology CRISPR to introduce the good mutations into the genome. “It is organic because no new DNA is introduced into the cells; rather we engineer in naturally occurring, benign mutations that are known to be beneficial to people with these conditions. It should prove to be a safe and effective therapy,” said Merlin Crossley, professor and deputy vice chancellor of UNSW, in a statement. “Our new approach can be seen as a forerunner to organic gene therapy for a range of common inherited blood disorders including beta thalassaemia and sickle cell anaemia.”