A New Therapeutic Approach for Brain Cancer through Zika?
First identified in Uganda in 1947, the Zika infection is a mosquito-borne disease which for most people, is a very mild infection and isn’t harmful. However, it may be more serious for pregnant women, as there’s evidence it causes birth defects – in particular, abnormally small heads (microcephaly).
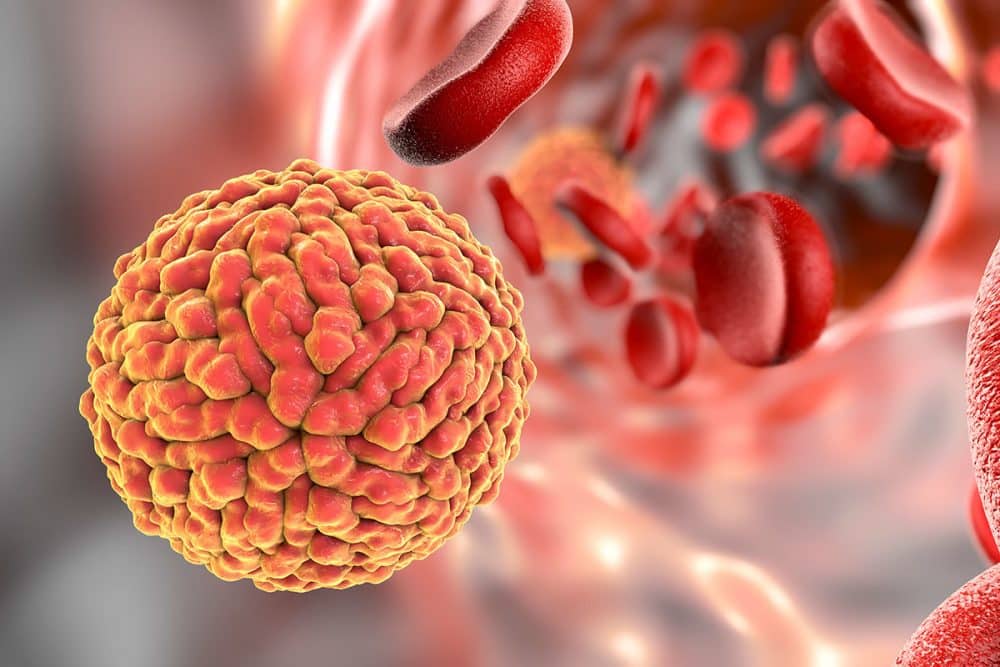
However, a recent study shows that the virus could represent an unlikely ally for treating glioblastoma. This is very welcome news, as glioblastoma is the most common and aggressive kind of malignant brain tumour in adults.
This discovery was made by researchers at the University of Campinas’s School of Pharmaceutical Sciences (FCF-UNICAMP) in São Paulo State, Brazil.
Previous studies have shown increased mortality rates for human progenitor cells, as well as growth inhibition and morphological abnormalities, in cells infected with Zika Virus. This is likely the cause of the observed microcephaly cases. The virus has also been shown to be capable of moving into brain cells, modifying the regulation of the cell cycle, and inducing their death.
In light of these findings, the researchers at FCF-UNICAMP set out to investigate the effects of Zika virus when it infects glioblastoma cells. To do this
, they infected human malignant glioblastoma cells with Zika and recorded microscope images of them 24 hours and 48 hours after infection in order to observe any metabolic alterations (cytopathic effects) caused by inoculation of the virus.
The results of the analysis showed that the glioblastoma cells displayed moderate cytopathic effects 24 hours after infection, such as rounded, swollen cell bodies and formation of syncytia, masses of cytoplasm in which the membrane contains several nuclei.
The most severe cytopathic effects were observed 48 hours after infection, with a larger number of rounded, swollen cells, more syncytium formation and pronounced loss of cell integrity, all of which denote cell death.
To identify the main compounds (metabolites) produced by glioblastoma cells during infection by Zika, the researchers analyzed the cells using matrix-assisted laser desorption/ionization mass spectrometry imaging (MALDI-MSI). The mass spectrometry data were submitted to statistical analysis, which showed that 24 hours after infection, the cells began to produce cardiac glycosides, especially digoxin.
Because digoxin and other cardiac glycosides have been shown to induce cancer cell death, the researchers concluded that infection by Zika triggered synthesis of the molecule in glioblastoma cells and that this phenomenon is probably one of the factors that lead to neuronal cell death. “Digoxin could be the key molecule that activates glioblastoma cell death during Zika infection,” said senior study investigator Rodrigo Ramos Catharino, Ph.D., a professor at FCF-UNICAMP and head of the institution’s Innovare Biomarker Laboratory.
Based on these findings, the researchers suggest that a genetically engineered Zika virus could eliminate the effects of infection and leave only the viral particles that synthesize digoxin.