Immune-Mimicking Scaffolds to Amplify T cell Expansion Increasing the Efficiency of Cancer Therapies
Therapeutic ex vivo T-cell expansion is limited by low rates and T-cell products of limited functionality. A new study at the Harvard Wyss Institute has now described a system that mimics natural antigen-presenting cells (APCs) thereby stimulating T cell growth and survival.
In a normal immune response, a type of white blood cell known as T cells are instructed by another kind of immune cell called an antigen-presenting cell (APC) to expand their numbers and stay alive. Adoptive cell transfer procedures are mimicking exactly this process in a culture dish by taking T cells from patients, multiplying them, sometimes genetically modifying them, and then returning them to patients so that they can, for example, locate and kill cancer cells.
However, these procedures often take weeks to produce batches of therapeutic T cells that are large and reactive enough to be able to eliminate their target cells.
With an APC-mimetic biomaterial scaffold, the researchers achieved greater expansion of primary mouse and human T cells than with existing methods; and they demonstrated the approach’s potential in a mouse lymphoma model treated with chimeric antigen receptor-expressing T cells (CAR-T cells) that are
engineered to home in on and destroy lymphoma cells.“Our approach closely mimics how APCs present their stimulating cues to primary T cells on their outer membrane and how they release soluble factors that enhance the survival of the T cells. As a result, we achieve much faster and greater expansion. By varying the compositions of lipids, cues, and diffusible factors in the scaffolds, we engineered a very versatile and flexible platform that can be used to amplify specific T cell populations from blood samples, and that could be deployed in existing therapies such as CAR-T cell therapies,” said David Mooney, Ph.D., a Core Faculty member at the Wyss Institute and leader of its Immunomaterials Platform.
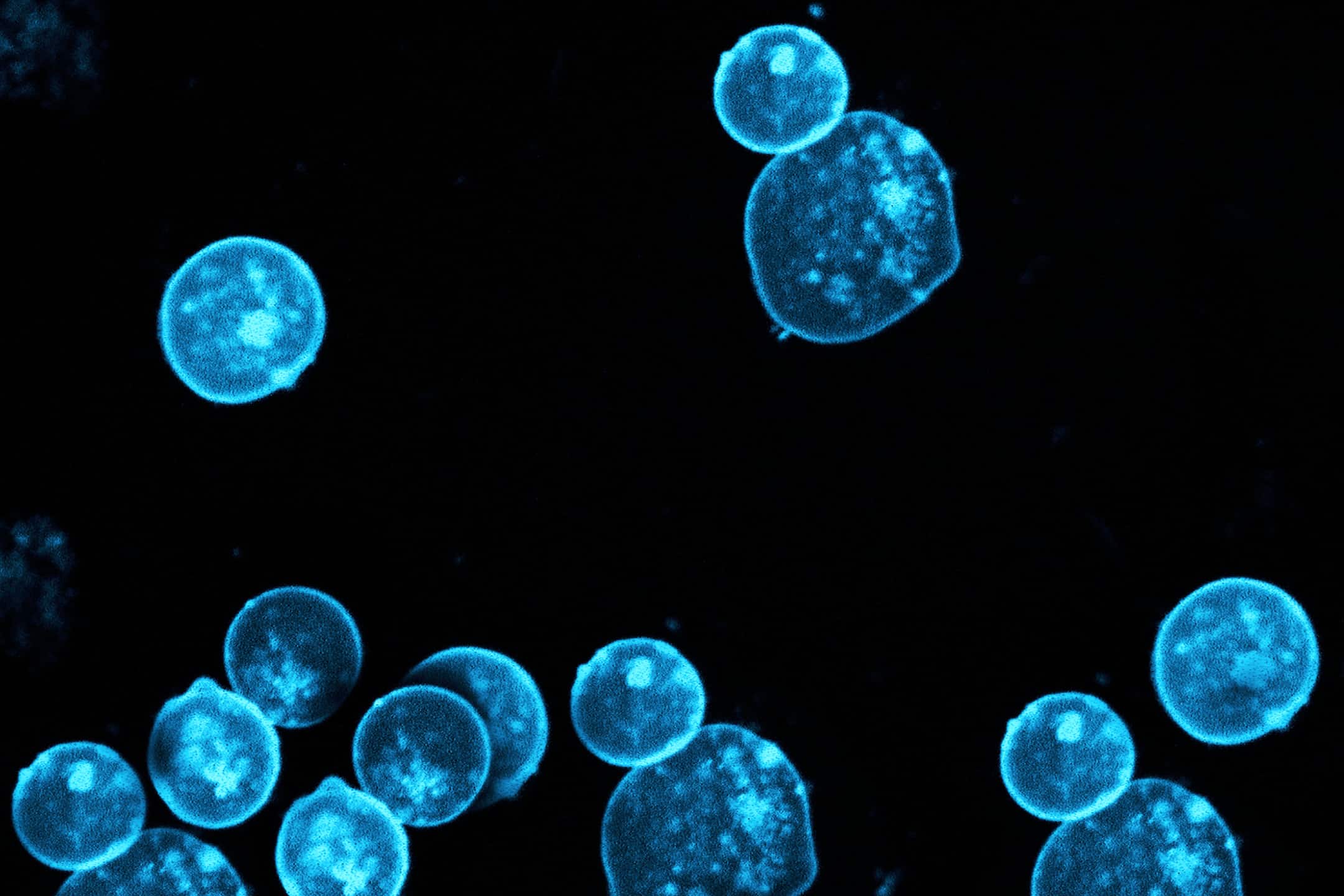
The scaffold was engineered using tiny mesoporous silica rods (MSRs) with Interleukin 2 (IL-2) being loaded, the MSRs were then coated with lipids that formed a thin supported lipid bilayer (SLB), which resembles the outer membrane of APCs and that the researchers then functionalized with a pair of T cell-stimulating antibodies that remain mobile in the lipid layer and can bind to receptor/co-receptor molecules on the surface of T cells.

The 3D scaffolds spontaneously formed in the culture medium through the settling and random stacking of the rods, forming pores big enough to allow the entry, movement, and accumulation of T cells, thereby signaling them to multiply. In a series of side-by-side comparisons, Mooney’s team demonstrated that APC-mimetic scaffolds performed better than methods involving commercially available expansion beads (Dynabeads), which are currently used in clinical adoptive cell transfer approaches.
“In a single dose, APC-mimetic scaffolds led to two- to ten-fold greater expansion of primary mouse and human T cells than Dynabeads. As another advantage, APC-mimetic scaffolds enabled us to tune the ratios of subpopulations of T cells with different roles in the desired immune responses, which in the future might increase their functionality,” said David Zhang, the study’s second author and a Graduate Student working with Mooney.
After successfully using the material to expand all T cells present in a sample, the team demonstrated that APC-mimetic scaffolds could also be used to expand antigen-specific T cell clones from a more complex mixture of cells.
Such T cell clones are constantly developed by the immune system to recognize small specific peptides contained in foreign proteins. To this aim, the researchers incorporated molecules into the scaffolds that are known as the major histocompatibility complex (MHC) and that presented small peptides derived from viral proteins to T cells.
“The bioinspired T cell-activating scaffolds developed by the Wyss Institute’s Immunomaterials Platform could accelerate the success of many immunotherapeutic approaches in the clinic, with life-saving impact on a broad range of patients, in addition to advancing personalized medicine,” said Wyss Institute Founding Director Donald Ingber, M.D., Ph.D., who is also the Judah Folkman Professor of Vascular Biology at HMS and the Vascular Biology Program at Boston Children’s Hospital, as well as Professor of Bioengineering at SEAS.