Pathway to Muscle Paralysis in Fatal Muscle Degeneration Disease
ALS—the disease popularly associated with Lou Gehrig, Stephen Hawking, and the Ice-Bucket Challenge- is a neurodegenerative disease affecting more than 20,000 adults in the US alone. Its hallmark symptom is muscle paralysis, which results when nerves decay and stop sending messages to muscles. When the breathing muscles lose connection with their controlling neurons, the respiratory system fails and the patient dies; in nearly half of ALS cases, this happens within three years.
Watching paralysis take hold of someone with ALS is like watching a massive stroke in slow motion. It starts with discrete problems in some fast-twitch muscle fibers, which grow weak, breakdown, and eventually stop working altogether. A person with minimal symptoms knows that they will become paralyzed and that the progression will be rapid and fatal.
The degree to which neurological conditions are terrifying has to do with how they mix certainty and mystery, and it’s rare to find a disease that brings them in worse proportions than ALS. The average life expectancy after diagnosis is three years. In that window, the immune system effectively switches from defending against
a foreign process to destroying the self.The unpredictability of ALS has long been in whom it’s going to affect. As we learn more about the disease, its complexity only grows. Doctors practicing medicine today were taught that ALS is a disease of motor neurons. This turns out to be true, but very incomplete: It is also a disease of protein clumping, and one facilitated by other cells in the nervous system. Scientists have only recently come to understand that what we currently call ALS acts through many different types of cells.
And now, researchers at the University of Arizona have taken an essential step forward in the quest to find the cause of amyotrophic lateral sclerosis. In the cells of flies, mice and humans with ALS, scientists at the UA have pinpointed a process that collapses when a critical protein’s blueprint is arrested on its way to protein construction.

A protein, TDP-43, previously had been identified as a common denominator in cases of ALS. “We are very interested in identifying the RNA molecules processed by TDP-43. In cases of ALS, RNA is not processed correctly, and that leads to motor neuron dysfunction,” says Daniela Zarnescu, professor in the department of molecular and cellular biology.
The team, in the course of their study, used fruit flies as a model organism to unravel the molecular pathways inside the cell and identified another protein- Hsc70-4 chauffeured by TDP-43, which was found to helping nerves communicate efficiently muscles.
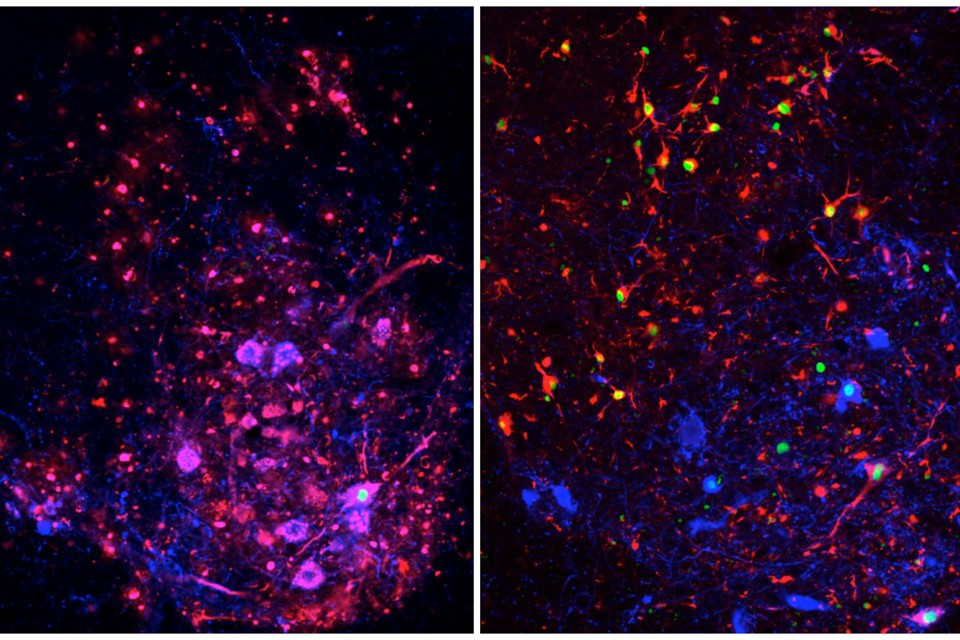
A mutation in TDP-43’s gene caused the flies to produce a higher-than-normal amount of the TDP-43 protein. Coyne found that flies producing more TDP-43 produced less of the protein Hsc70-4, suggesting that excess TDP-43 prevents the creation of Hsc70-4.

A doctoral student in Zarnescu’s lab, Alyssa N. Coyne, found that the mutation generates too much TDP-43, and also predisposes the protein to form aggregates, which are clumps of protein that cling to RNA. And as a result- if the RNA encoding Hsc70-4 cannot move, then the cell cannot use it to make the Hsc70-4 protein. Coyne discovered that without enough Hsc70-4, the flies took more time to right themselves after being rolled onto their backs — a sign that the flies’ nerve cells were slow to communicate with their muscles. Her next step was to identify what role Hsc70-4 plays in that communication.
Muscles move when they receive messages from their controlling nerves in the form of neurotransmitters. Vesicles — the shipping containers of the cell — filled with neurotransmitters move to the end of the nerve cell, where they release their contents into the gap between nerve and muscle. Then, the vesicles are pulled back into the nerve cell and refilled. This process is called the synaptic-vesicle cycle, and its efficiency is crucial to the quick communication between nerve and muscle. Coyne found that Hsc70-4 is responsible for ensuring this efficiency, as it works at the cell membrane to release and retrieve vesicles.
“If you don’t make the correct amount of this protein, then the synaptic-vesicle cycle will be less efficient. With time, this process will deteriorate, and that could potentially lead to the pulling away of the motor neuron axon from the muscle and paralysis,” Zarnescu said.
“We validated our findings of decreased synaptic Hsc70 in mouse neurons as well as patient derived neurons,” Coyne said.
Coyne said that the study is particularly valuable as it identifies novel targets and pathways that could be used for development of future ALS treatments.