PuLMo: An Artificial Lung in Development for Safe Drug Testing
The human body on a microchip may be the future of biomedicine. Scientists all over have already begun to develop micro-scale models of organs such as the heart, lungs, and liver. The aim is to replace testing on animals and improve the accuracy of the models. One of such researches involves a team of scientists at the Los Alamos National Laboratory who have developed a tissue-engineered artificial lung called PuLMo, for Pulmonary Lung Model that simulates the response of the human lung to drugs, toxins, particles and other agents.
The marriage of microsystems technology with life sciences is described as a revolution in the field of biomedicine. It is a rapidly growing area, offering new tools and more accurate models as we try to understand the body’s various organs. Ultimately, it may lead to new and better therapies for a wide variety of diseases.
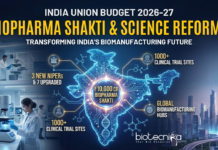
Under the ATHENA research program, the Defense Threat Reduction Agency within the U.S. Department of Defense has funded work integrating miniature artificial hearts, livers, lungs and kidneys into surrogate human organ systems.
The agency supports this work to help develop countermeasures to chemical or biological warfare threats. In the early development phases, those countermeasures can’t ethically be tested on human populations.
So these surrogate organs, which mimic the function and response of actual human organs, address a crucial problem: accurately predicting how humans will respond to a drug or toxin. For decades now, drug trials have relied on animals. Some drugs have passed animal trials only to fail — sometimes fatally — in human trials. A new lung model will allow researchers to observe a drug’s effects without endangering human subjects.
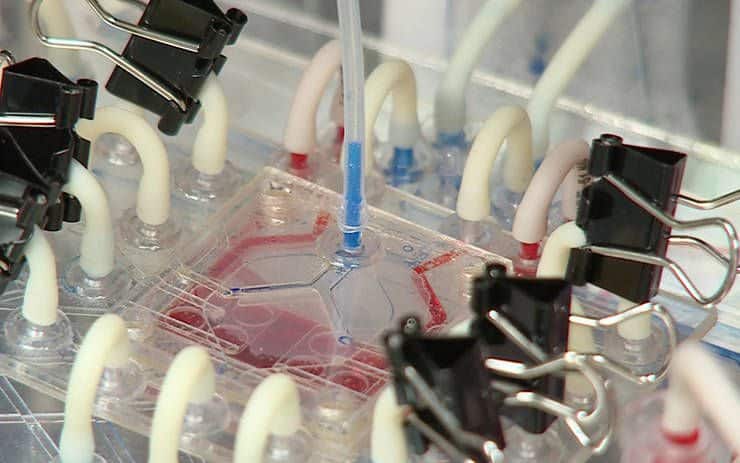
PuLMo consists of a bronchiolar unit and an alveolar unit. They work the way a lung is supposed to work — PuLMo breathes. A microfluid circuit board manages the flow of fluids and air through each plastic unit. When cells are placed in PuLMo and fed the proper environment, they flourish as they would in the body.
And owing to the artificial organ’s flexibility in accommodating a variety of cell types and tissues, PuLMo can can test a wide range of conditions just by tweaking the variables, such as tissue and cell types, a drug, or a pathogen, one at a time. Since it can be configured to suit the experiment, researchers decide which cells they want to study in mixed populations, an approach that’s faithful to how the human body works but difficult when cultures are isolated in a Petri dish. Every tissue in the body has multiple cell types, and they all provide nutrients and signals to each other. PuLMo replicates those conditions.
Combined with PuLMo’s exciting and far-reaching potential to raise the reliability of drug-toxicity assessments and predicting how new pharmaceuticals will perform in humans, PuLMo has the potential to save time, money, and — most crucially — lives, whether they are soldiers or citizens.