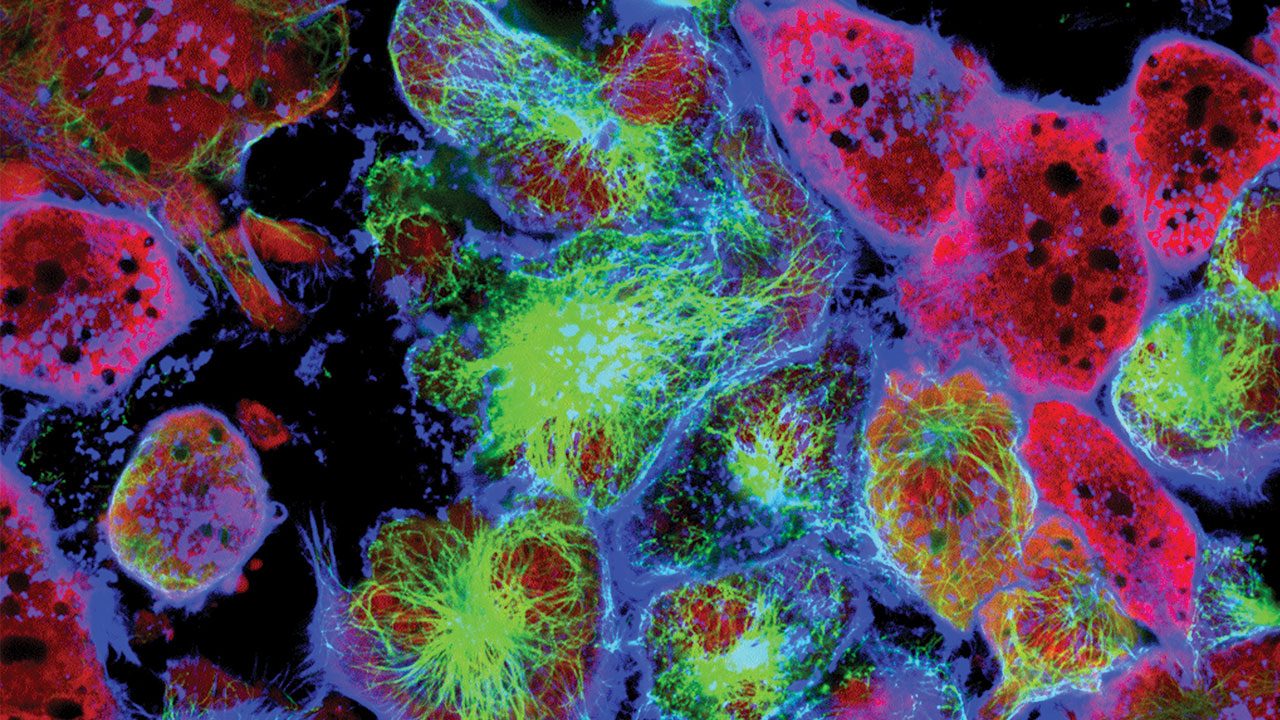
Cancer Drug developed by researcher,shows Potential in Treating Tumours
Targeted therapy, as the name suggests, involves the use of ‘designer molecules’ directed against a particular rogue molecule in the body that is responsible for cancer. Targeted therapy stops the action of molecules that are key to the growth of cancer cells. Thus, it affects cancer cells more so than normal cells. Targeted therapy’s specific action differs from traditional chemotherapy, which affects all fast-growing cells.
Many such molecules have found phenomenal success as effective cancer drugs in recent years. The latest discovery from Prof. Sathees Raghavan’s group at the Department of Biochemistry, Indian Institute of Science, Bangalore, in collaboration with researchers from various other institutes, is a noteworthy addition to this list of molecules.
Designed and synthesised by researchers from eight different research groups spread over labs in Mumbai, Thiruvananthapuram, Bengaluru, and with contributions from a couple of Indian scientists at the Department of Molecular and Clinical Cancer Medicine, University of Liverpool, Disarib belongs to the class of “designer molecules” that zero in on rogue cells as part of the targeted therapy method to combat cancer.
The molecule (Disarib) binds to a protein BCL2 and inhibits the protein from suppressing cell death in cancer cells. While BCL2 protein is produced in excess in cancer cells, its expression is almost undetectable in normal cells. Hence, Disarib targets and kills only cancer cells while sparing normal cells.
BCL2 is a regulator protein molecule found in our cells. Its primary job is to suppress a process called apoptosis– a method of programmed cell death. This suppression is important since we don’t want our cells to simply die. However, when our cells are diseased or worn out, then apoptosis becomes necessary.
In cases where apoptosis fails, when our body cannot get miscreant actively-dividing cells to commit suicide, that’s when the cells become pathogenic and turn cancerous. And BCL2, as an apoptosis inhibitor, helps them do just that. Hence, targeting BCL2 may be a clever idea to control the progression of cancer. “BCL2 is an attractive drug target because many different cancers, including a lot of chemo and radiotherapy resistant ones, over produce BCL2”, explains Prof. Raghavan. “The normal cells in our body, in contrast, make very less BCL2. Drugs designed to inhibit BCL2 thus affect only cancer cells and little else”, he adds.
Inside a cell, there is always a balance between proteins that promote cell death (apoptosis) and those that suppress cell death. Since the proteins (BAX and BAK) that promote cell death get bound to BCL2, normal cell death is suppressed and cancer cells are able to live longer. The team, in this case, was able to disrupt the interaction of BCL2 and apoptosis-causing BAK protein and cause the death of cancer cells.
The efficiency of Disarib to cause cell death and tumour regression was far superior compared with the FDA-approved ABT199. Prof. Raghavan says preliminary studies by his group show that the home-grown molecule gets better results than the one approved by the FDA in terms of elimination of cancer cells. And, it does so in significantly smaller doses, reducing further the chances of side effects. “The smaller size of the Disarib molecule, compared with ABT199, makes it easier for the drug to reach the cancerous cells where it can begin destroying the tumour,” adds his colleague Supriya Vartak. The results have been published in Biochemical Pharmacology.
Unlike ABT199, the small molecule binds predominantly to a different domain (BH1) of BCL2 and showed better efficiency in killing cancer cells. Furthermore, compared with ABT199 inhibitor, the small molecule synthesised by the team did not cause any side effects.
The researchers have left no stone unturned during the study of Disarib, including its mechanism of action. Following a number of preliminary testing and analyses, the drug was tested in cancer cell lines, animal models, patient samples and more. The team even successfully utilized a humanized model of tumour in mice for ovarian carcinoma, in addition to three independent mouse tumour models for investigating the tumour regression property of Disarib.
And soon, cancer biologists, chemists, clinicians, and specialists in bioinformatics, belonging to different labs, will be pooling in their expertise in the area in order to carry out pre-clinical tests of the drug, under the multi-crore rupee project titled ‘Glue Grant’.
The Department of Biotechnology (DBT), New Delhi, has approved this collaborative effort to produce the first home-grown drug. Pharmaceutical companies have shown some interest, which is very encouraging, says Prof. Raghavan, though he cautions that results of the study approved by the DBT will decide when the drug will be available in the market.