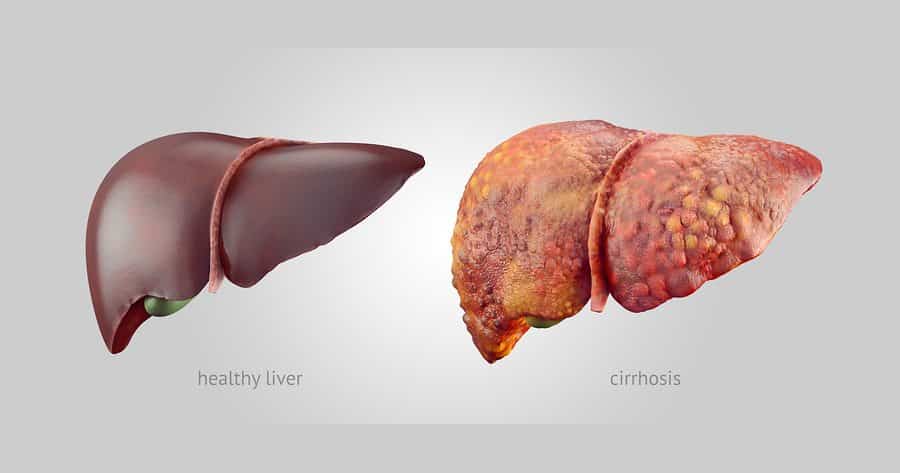
IBM Taps Machine Learning to Access Cirrhosis Mortality Rates
Accurate assessment of the risk of mortality following a cirrhosis-related admission can enable health-care providers to identify high-risk patients and modify treatment plans to decrease the risk of mortality.
And now, a new research from IBM using electronic health record data and a new risk scoring process supported with machine learning technology is being used to generate a post-discharge mortality prediction model for patients with a cirrhosis-related admission.
Nine variables are the most effective predictors for 90-day mortality, which can save lives, researchers note in a study available here. The predictors include total bilirubin, creatinine, albumin, INR, WBC, length of stay, age, sodium and total cholesterol.
Researchers created a post-discharge mortality prediction model for patients with cirrhosis receiving care at Massachusetts General Hospital or Brigham and Women’s Hospital between 1992 and 2010, then identified 4,781 cirrhosis-related admissions at the hospitals—of which 778 resulted in death within 90 days of discharge.
Inspired by other studies led by Harvard’s Informatics for Integrating Biology and the Bedside (i2b2) group, the researchers at IBM took an unbiased approach toward the discovery of
biomarkers. In this approach, a feature-selection machine learning algorithm observed a large collection of health records and identified a small set of variables that could serve as the most efficient predictors for a given medical outcome.They used the well-studied supervised learning paradigm to assess accuracy; they also applied traditional statistical methods to assess the validity of our approach. They then realized that by combining the components of MELD (or the components of its extended version MELD-Na) with several easily accessible variables, we could construct a new score that was approximately 10 percent more accurate. They referred to our new score as “MELD-Plus.”
The study used a new risk score called Model for End-Stage Liver Disease (MELD)-Plus—an improvement of earlier versions of the MELD score. By applying the new risk score, out of an independent data source of 24,042 cirrhosis-related admissions (of a total of 18,345,793 individuals), MELD-Plus outperformed the earlier versions of MELD by approximately 10 percent.
MELD scores are important as they help prioritize patients and determine which patient is the next on the waiting list to get a new liver, says Uri Kartoun, a co-author of the study and a research staff member at IBM.
“Think of a hypothetical gastroenterology department at a hospital that provides care to some 100 patients with an advanced liver disease,” Kartoun explains. “Since there are much more patients who need a new liver vs. available livers, the clinicians need to rank the patients according to their level of urgency for a liver transplantation. Since 2002, the United Network for Organ Sharing has used MELD which is a simple equation capable of ranking such patients and determine their place on the liver transplantation waiting list.”
Increased maturation of electronic health records, easier and faster accessibility to data and new statistical and machine learning algorithms developed in recent years made it possible to create MELD-Plus which more accurately determine the next patient in line, compared to the original MELD score. “I don’t know how to assess that yet, but I think that MELD-Plus could extend the total life expectancy of those 100 hypothetical patients,” Kartoun contends.