Turning on the Gene “Circuit” Switch to Combat Cancer
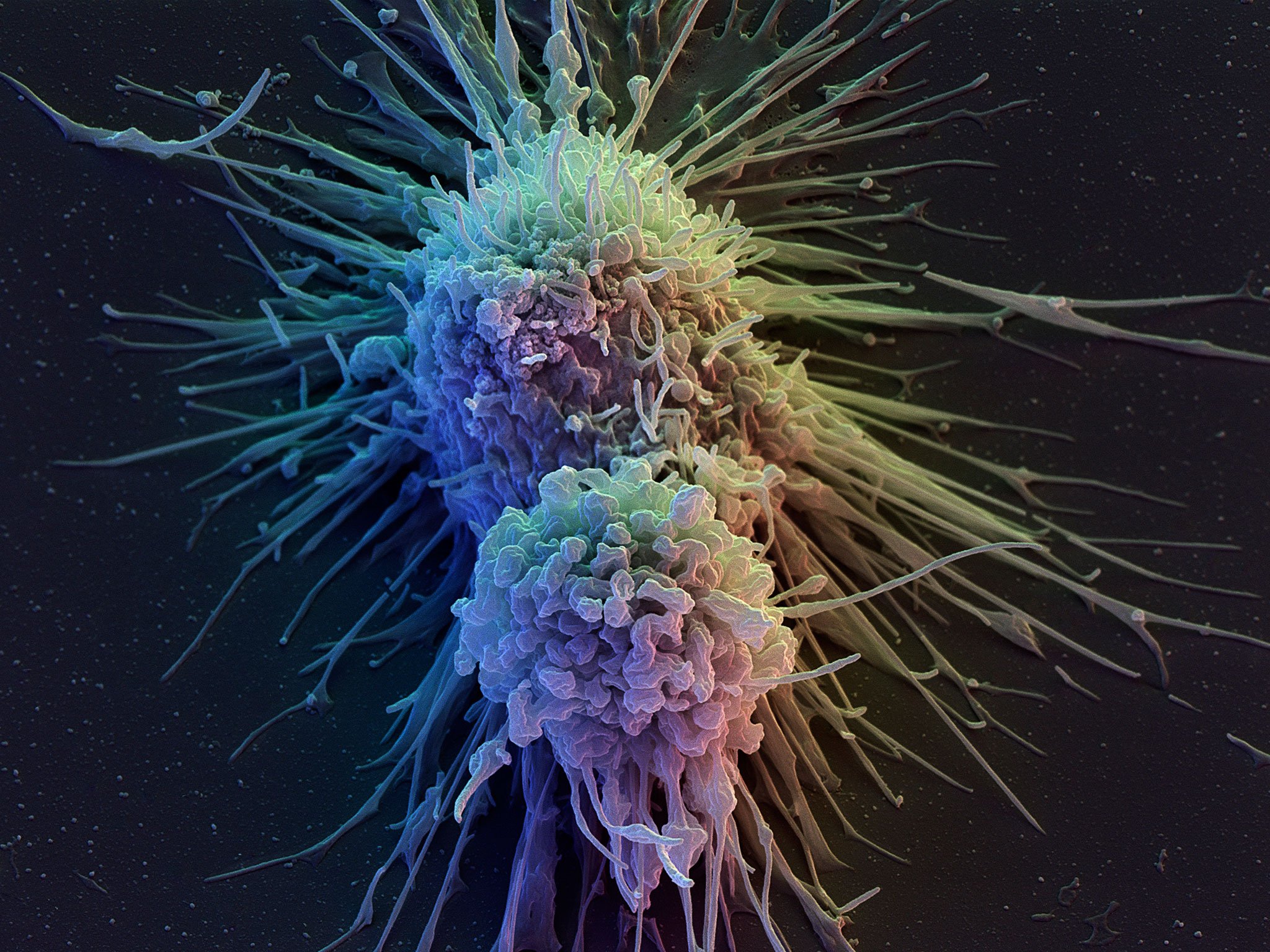
Despite its success in several clinical trials, cancer immunotherapy remains limited by the rarity of targetable tumor-specific antigens, tumor-mediated immune suppression, and toxicity triggered by systemic delivery of potent immunomodulators.
Therefore, scientists at the MIT have now found an alternative strategy to win over cancer- by switching on the synthetic gene circuits inside these cells, thereby triggering the immune system to finish them off.
“There has been a lot of clinical data recently suggesting that if you can stimulate the immune system in the right way you can get it to recognize cancer,” says Prof. Timothy Lu, who’s head of the Synthetic Biology Group in MIT’s Research Laboratory of Electronics. “Some of the best examples of this are what are called checkpoint inhibitors, where essentially cancers put up stop signs [that prevent] T-cells from killing them. There are antibodies that have been developed now that basically block those inhibitory signals and allow the immune system to act against the cancers.”
The research team in this study believes that there is a need to develop more specific and localized immunotherapies instead of treating the body systemically. They are also interested in including multiple immunotherapies in a single package that can stimulate the immune system in several ways rather than just one, in case of cancer adapting to treatment.
To achieve this, Dr. Lu’s MIT team has created a gene circuit encoded in DNA which is designed to detect cancerous and noncancerous cells. The circuit can also be customised to respond to different kinds of tumors and uses the same principle that AND gates in electronics use. These biological AND gates only switch on the circuit when the two specified inputs are detected.
This customized circuit is delivered to local cells in the affected region of the body using gene therapy. The synthetic promoters then bind to target proteins that are present only in tumor cells, causing the promoters to activate.
The DNA circuit itself only switches on when two of these cancer promoters are activated. This means the circuit can specifically target tumors with higher accuracy than existing therapies, and it is safer because it requires two cancer-specific inputs to activate the circuit.
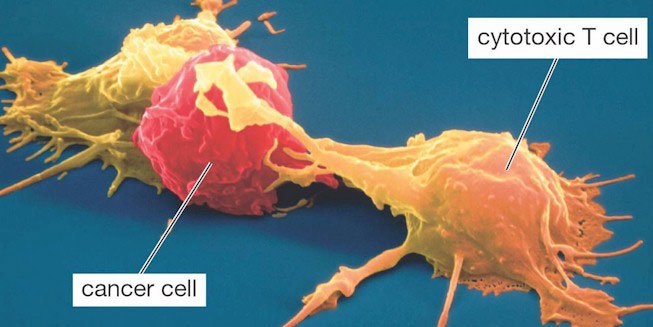
When the circuit is activated, it secretes proteins that attract the cells of the immune system and directs them to attack the tumor cells. This includes surface T cell engagers, which direct the T Cells to destroy the cancer cells. Additionally, the circuit expresses a checkpoint inhibitor that removes the barrier to T cell activity, allowing it to spot the cancer cells and move in for the kill.
When the researchers tested the circuit during in vitro studies, they discovered it was able to detect ovarian cancer cells hiding among healthy ovarian cells and even other cell types.
Lu affirmed that the researchers had identified other breast cancer selective promoters, and once encoded into the circuit, breast cancer cells would be targeted by these promoters over other cell types.
Eventually, researchers hope that the circuit will be also used in targeting other diseases like inflammatory bowel disease, rheumatoid arthritis, and other autoimmune diseases.