Scientists Implant Stem-Cell-Derived Small Bowel Segments Into Rats
Short bowel syndrome (SBS) is the end-stage pathology of various gastrointestinal disorders, including Crohn’s disease, mesenteric ischemia, and midgut volvulus. Affected patients develop intestinal failure when the remaining bowel no longer has sufficient absorptive capacity to allow for enteral nutritional autonomy, and patients become dependent on intravenous nutrition for maintenance.
Small bowel transplantation is now accepted worldwide as a treatment option for patients with irreversible intestinal failure. In 2015, a total of 127 intestinal transplantations were performed in the U.S., but an additional 275 patients remain on the wait list due to a shortage of suitable organs. Although early-term graft survival has improved over the past decade, graft failure rate at 3 years remains high at 41.9% for transplants in 2009–2010. A recipient’s evoked immune response to the allograft often results in acute cellular rejection and chronic allograft enteropathy. Even when effective, life-long immunosuppression has numerous complications, including opportunistic infections, renal dysfunction, and lymphoproliferative disorders.
Now, a research team at the Massachusetts General Hospital has bioengineered functional small intestine segments that, when implanted into rats, were capable of delivering nutrients into the bloodstream.
“In this study we have been able to bridge the gap between differentiation of single cells – driving stem cells to become a specific cell type – and the generation of tissue that shows a higher level of function – in this instance vascular perfusion and nutrient absorption,
” says Harald Ott, MD, of the MGH Department of Surgery and the Center for Regenerative Medicine, senior author of the report. “While previous studies have reported successful differentiation of organoids – millimeter-small units of tissue – from iPSCs, we describe a technology that enables these smaller units of tissue to form larger-scale grafts that someday could be used as implanted replacement organs.”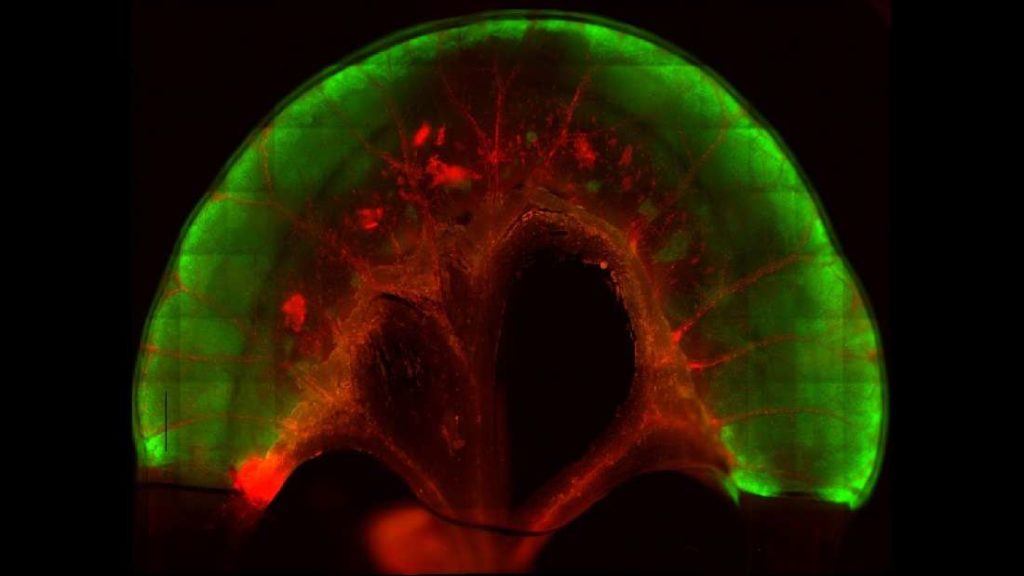
The procedure involves stripping the living cells from a donor organ with a detergent solution and then repopulating the remaining extracellular matrix scaffold with organ-appropriate types of cells. The team decellularized 4 cm segments of rat small intestine and confirmed the applicability of the procedure to larger animals in segments of pig intestine.
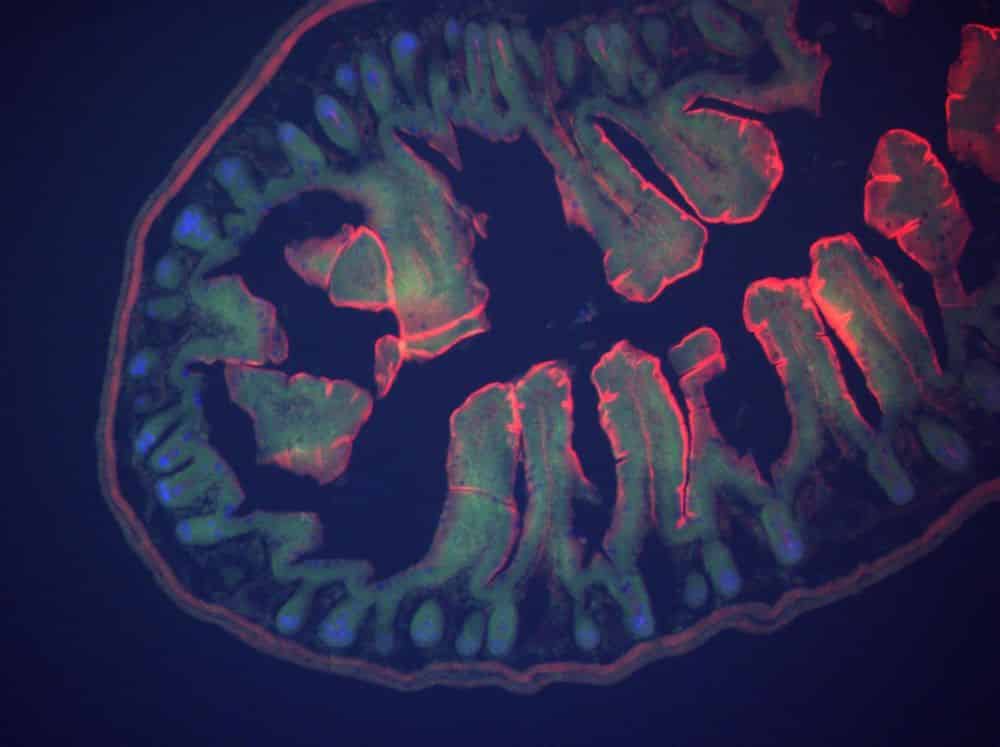
While the decellularized small intestine would provide the structural scaffold for both the complex tissue of the interior lining and the vascular channels, repopulating the scaffold requires the delivery, engraftment and maturation of two types of cells – epithelial cells for the intestinal lining and endothelial cells for the blood vessels – in the right locations. Generation of epithelial tissue began with human iPSCs that were differentiated into intestinal precursor cells and then seeded into the interior of the decellularized segments, which then were cultured. Two weeks later, after formation of the epithelial layer, human endothelial cells were seeded into the vascular channels; and the segments placed in a perfusion bioreactor system for further maturation.
Several days later, in vitro testing of the segments confirmed blood passage through the repopulated vasculature and showed that the reconstituted intestinal tissue could transfer glucose and fatty acids from the interior of segments into the blood vessels. The repopulated epithelial cells lining the segments had the same polarized structure – with the proteins lining cellular membranes on the interior of the segments differing from those at the base of the cells – seen in naturally occurring intestinal epithelium.
A few of the segments were sutured to the carotid arteries and jugular veins of immunodeficient rats. The vasculature of the segments was immediately perfused with blood, and four weeks later injections of either glucose or fatty acids into the segments resulted in increased levels in the animals’ bloodstreams, confirming absorption of the nutrients. In addition, specific types of cells normally found in the intestinal lining that had not appeared while the segment were cultured did after implantation into the living animals, implying continued maturation of the tissue.
“Our in vivo experiments showed that human iPSCs differentiated towards an intestinal fate can be assembled into an intestinal graft with a high level of organization and connected to a recipient’s vasculature to enable nutrient absorption after transplantation,” says Ott, who is an associate professor of Surgery at Harvard Medical School. “The next steps will be to further mature these grafts and to scale the construct to a human size, so that someday we may be able to provide a more accessible alternative to small bowel transplantation for patients with short bowel syndrome – ideally growing ‘on-demand’ patient-specific grafts that would not require immunosuppressive drugs.”