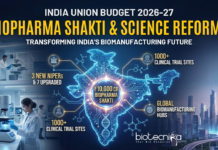
Ablynx’s Dangerous Blood Disorder Treatment – Hercules
The Belgian biotech, Ablynx has now chalked up a big win with its lead candidate caplacizumab for a rare blood disorder, acquired thrombotic thrombocytopenic purpura (aTTP) reporting positive phase III data.
In July, caplacizumab received FDA fast track status for treating thrombotic thrombocytopenic purpura (aTTP), an orphan blood disease affecting 7,500 US Americans per year. Now, Ablynx (Ghent) announced that the bivalent antibody, which targets the von Willebrand factor (vWF) in order to prevent formation of platelet micro-clots that cause the severe thrombocytopenia, tissue ischemia and organ dysfunction in aTTP, met the primary and certain secondary endpoints in the pivotal Hercules Phase III study, which enroled 145 patients.
Caplacizumab is a bivalent anti-vWF Nanobody that received Orphan Drug Designation in Europe and the United States in 2009. Caplacizumab blocks the interaction of ultra-large vWF multimers (ULvWF) with platelets and, therefore, has an immediate effect on platelet aggregation and the ensuing formation and accumulation of the micro-clots that cause the severe thrombocytopenia, tissue ischemia and organ dysfunction in aTTP. This immediate effect of caplacizumab has the potential to protect the patient from the manifestations of the disease while the underlying disease process resolves.
Top-line results showed that treatment with caplacizumab resulted in a significant reduction in time to platelet count response, the primary endpoint of the study. Ablynx noted that patients on caplacizumab were 1.5-times more likely to achieve platelet count response at any given time point, compared to those treated with placebo.
Caplacizumab’s effect on the percentage of patients with aTTP-related death, recurrence of aTTP or one or more major thromboembolic event landed in the success column. The clinical trial linked Ablynx’s drug to a 74% drop in these events, primarily because it outperformed placebo in terms of its effect on recurrences.
That effect on the rate of recurrences was reflected in the other successful secondary endpoint. The proportion of patients with a recurrence of aTTP was 67% lower in the caplacizumab cohort, resulting in the trial hitting that secondary endpoint.
The safety data echo those from the phase 2. As in that trial, more patients in the phase 3 who took the study drug experienced bleeding-related adverse events—66.2% versus 49.3%— but most cases were of mild to moderate severity.
“Patients with aTTP are at risk for significant morbidity and early death. We believe these positive Phase III study results confirm the potential for caplacizumab to address the high unmet medical need in the treatment of aTTP and to have a meaningful impact on the lives of affected patients. We continue to analyse the data and look forward to sharing the results with regulatory authorities and the scientific community.” Dr Robert K. Zeldin, Chief Medical Officer at Ablynx, commented. “We thank the study participants and their families as well as the investigators and staff who contributed to this study.”
Dr Edwin Moses, CEO of Ablynx, said, “I am delighted by this outcome as it reinforces all our beliefs in the potential for caplacizumab to change the lives of patients affected by aTTP. This is a very important milestone for the Company as it further validates our Nanobody platform and demonstrates our ability to discover and develop medicines that make a real difference for society. These results strengthen our resolve to obtain marketing approval as quickly as possible so that caplacizumab rapidly becomes available to patients suffering from this severe disease for which there is currently no approved drug available.”
“The results of this landmark trial constitute a complete game changer for patients with aTTP. They will revolutionise how we manage the acute phase of the disease, which is when patients are at highest risk for organ damage, recurrence and death.” Said Professor Marie Scully, leading TTP specialist from the University College Hospital in London and Investigator in the HERCULES study.