Using a combination of immune-checkpoint inhibition and plasmonic gold nanostar (GNS)–mediated photothermal therapy, scientists at the Duke University, have now been able to achieve complete eradication of primary treated tumors and distant untreated tumors in some mice implanted with the MB49 bladder cancer cells.
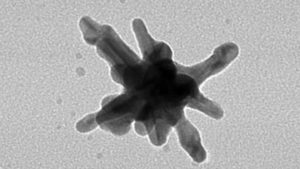
Their study involving SYMPHONY, Synergistic Immuno Photothermal Nanotherapy, injects gold nanoparticles into the bloodstream, these star-shaped nanoparticles (nanostars) then accumulate in tumors after circulating within the blood. Further, the tumor is blasted with a laser, causing the nanoparticles to heat up and burning the tumor.
The team combined the nanostar treatment with an FDA-approved immunotherapy that acts to help the body’s immune system destroy cancer cells. By combining the immunotherapy and the nanostar technique, the team hoped that they could achieve better results than with either approach alone, and also target tumors at distant sites, called metastases.
The new approach relies on a “photothermal immunotherapy” technology developed by an interdisciplinary group of Duke researchers that uses lasers and gold nanostars to heat up and destroy tumors in combination with an immunotherapeutic drug. This photothermal therapy hinges on the widely demonstrated fact that nanoparticles accumulate preferentially within a tumor due to its
leaky vasculature.“The nanostar spikes work like lightning rods, concentrating the electromagnetic energy at their tips,” said Tuan Vo-Dinh, a researcher at Duke University. “We’ve experimented with these gold nanostars to treat tumors before, but we wanted to know if we could also treat tumors we didn’t even know were there, or tumors that have spread throughout the body.”
Cancer is a severe threat to human life and results in more than 7 million deaths each year. Many cancers exploit immune checkpoints to evade the anti-cancer immune response. Immune checkpoint inhibition is a promising immunotherapy that aims to reverse signals from immunosuppressive tumor microenvironments.
Dr. Vo-Dinh explained that the body’s immune system protects against the growth of
cancerous cells. Many tumors, however, overproduce the programmed death-ligand 1 (PD-L1) molecule, which disables T cells so they cannot attack the tumor. A number of drugs are being developed to block the action of PD-L1.
In the study, the Duke team injected bladder cancer cells into both hind legs of a group of mice. After waiting for the tumors to grow, the researchers explored a number of therapies, but only on one of the legs.
Those that received no treatments all quickly succumbed to the cancer, as did those receiving only the gold nanostar phototherapy, because the treatment did nothing to affect the tumor in the untreated leg. While a few mice responded well to the immunotherapy alone, with the drug stalling both tumors, none survived more than 49 days.The group treated with both the anti-PD-L1 immunotherapy and the gold nanostar phototherapy fared much better, with two of the five mice surviving more than 55 days.
“When a tumor dies, it releases particles that trigger the immune system to attack the remnants,” said Dr. Vo-Dinh. “By destroying the primary tumor, we activated the immune system against the remaining cancerous cells, and the immunotherapy prevented them from hiding.”
According to Dr. Vo-Dinh, one mouse is still alive almost a year out with zero recurrence of the cancer. When more cancerous cells were injected, the mouse’s immune system attacked and destroyed them, demonstrating a vaccine effect in the cured mouse.
This was a proof-of-concept study, but the team plans to test the technique on other types of cancer and hopes that it might be useful in humans.