Rice University Team Explores CRISPR’s Sickle Cell Correction Potential
Sickle cell anemia is a genetic disease with severe symptoms, including pain and anemia. The disease is caused by a mutated version of the gene that helps make hemoglobin — a protein that carries oxygen in red blood cells. People with two copies of the sickle cell gene have the disease. People who carry only one copy of the sickle cell gene do not have the disease, but may pass the gene on to their children.
The mutations that cause sickle cell anemia have been extensively studied and demonstrate how the effects of mutations can be traced from the DNA level up to the level of the whole organism. Now, researchers at the Rice University claim to have used the CRISPR editing system to correct the sickle cell mutation in up to 40% of stem cells taken from affected patients.
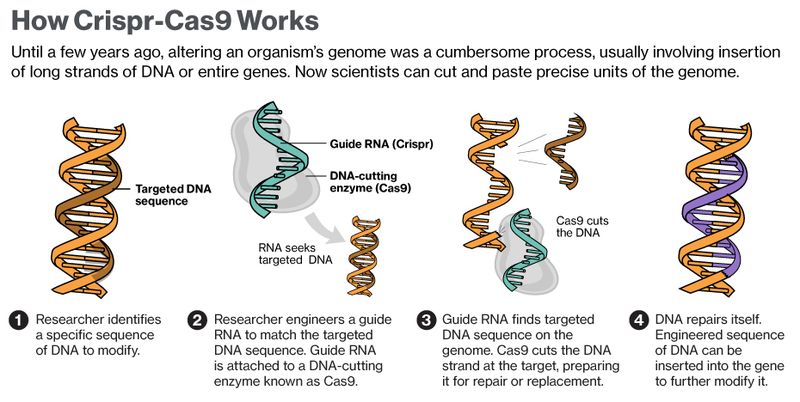
Rice University bioengineers have found new techniques for precision genome editing that are more accurate and have fewer off-target errors. Bioengineering Professor Gang Bao and his colleagues present ideas for maximizing on-target gene editing with biological catalysts capable of cutting DNA called “engineered nucleases.” Several such systems have been studied for years, but for the past three, the promise of cut-and-paste editing via CRISPR-Cas9 has captured the attention of scientists worldwide.
CRISPR-Cas9, a naturally occurring defense system in bacteria, allows researchers to design a short sequence of RNA called “guide RNA” that targets a specific section of genetic code (DNA) in a cell. An associated Cas9 protein then cuts the section, disrupts it or replaces it with the desired code.
And about three years ago, researchers discovered how bacterial CRISPR-Cas9 could be modified to edit DNA in human cells. But CRISPR-Cas9 is still vulnerable to snipping the wrong sequences – called “off-targets” – in addition to the right ones. In therapeutic applications, Bao said, off-target cutting by CRISPR-Cas9 could cause many detrimental effects, including cancer.
In the course of their study, the Rice researchers zeroed in on stem cells and progenitor cells, which can differentiate into a more limited range of cell types than stem cells: “Sickle cell disease is caused by a single mutation in the beta-globin gene. The idea is to correct that particular mutation, and then stem cells that have the correction would differentiate into normal blood cells, including red blood cells. Those will then be healthy blood cells,” Bao said.
“We still don’t know whether repairing as much as 40 percent of the cells is enough to cure a patient. We’d like to say, ‘Yes’ – but we don’t really know yet. That’s something we hope to learn from an eventual clinical trial,” Professor Gang Bao, of Rice University in Texas, told the American Association for the Advancement of Science annual conference in Austin.
Even if a 40 per cent success rate on cell repair turns out not to be enough, his work represents a step forward in the fledgling area of gene editing – although experts cautioned that much more research was needed before this became a viable treatment for people suffering from sickle cell disease.
Bao says there is a path forward, represented in part by his investigation of two new bacterial systems as well as the fact that CRISPR-Cas9 is a much easier technique to implement in the lab than other genome-editing systems such as TALEN and zinc finger nuclease.