Boosting Oestrogen Activity For New Neuroblastoma Treatment Possibility
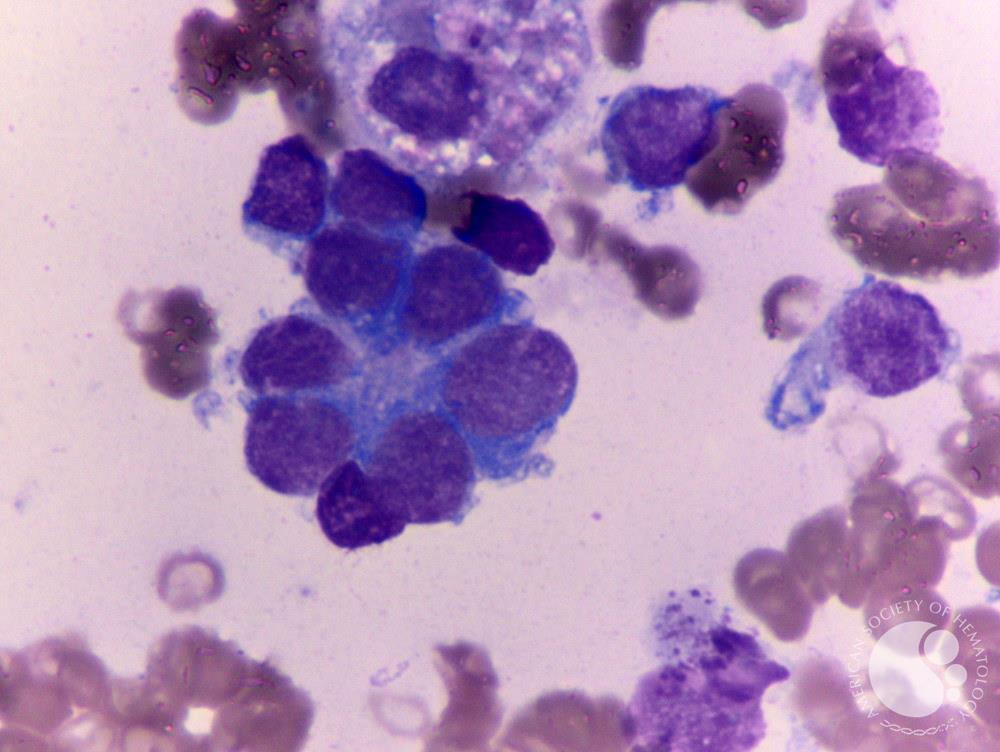
Neuroblastoma (NB), the most common solid malignant extracranial childhood tumor, develops from sympathetic precursor cells of neural crest origin. This form of cancer accounts for about 8–10% of all cases of childhood cancer and is the cause of 12–15% of cancer-related childhood mortality.
About half of the affected children have a localized low-risk disease while the other half is diagnosed with a metastatic high-risk NB. Even today, metastatic high-risk NB is difficult to cure despite multimodal therapy, resulting in a 5-y survival rate of around 50%.
“Our research focuses particularly on the activity of this gene and how it relates to neuroblastoma,” says Professor Marie Arsenian-Henriksson at the Department of Microbiology, Tumor and Cell Biology, Karolinska Institutet, who led the study that explored the role the female sex hormone in neuroblastoma. “MYCN is often seen only as a marker for a poor prognosis, but it’s critical to the disease and is a possible target for new drugs.”
Previously, Arsenian-Henriksson’s group found that the activation of MYCN led to the formation of microRNAs that disable ERalpha, the estrogen receptor. In this study, the scientists found that by inhibiting these microRNAs, neuroblastoma cells with MYCN activation could mature into neuron-like cells, which behaved more like normal cells.
They also found that an estrogen therapy in combination with an overexpression of the estrogen receptor could lead to the same result.
The researchers studied tumour tissue from patients, cultivated human tumour cells and tumours in mouse models for neuroblastoma. In the mice, the neuron-like cells did not grow as quickly as the original cancer cells, and analyses of the tumour tissue from patients show that those with a high level of the oestrogen receptor have a better survival rate that those with a low.
“Our data suggests that oestrogen could be a therapeutic method for patients who express high levels of the oestrogen receptor,” continues Professor Arsenian-Henriksson. “Another possible therapy could involve deregulating MYCN or upregulating the oestrogen receptor and then treating with oestrogen. We have previously shown that the deregulation of MYCN leads to a high expression of the oestrogen receptor.”